Interview Summary
For this article, EMJ interviewed Philippe Gevaert, who is a Professor in Rhinology and Allergy at the Department of Otorhinolaryngology in Ghent University, Belgium. Gevaert is a prominent figure in chronic rhinosinusitis and allergic rhinitis, having been involved in the European Rhinologic Society (ERS) and past-Chair of the ear, nose, throat (ENT) section of the European Academy of Allergy and Clinical Immunology (EAACI).
In this interview, Gevaert explores the pathogenesis of chronic rhinosinusitis with nasal polyps (CRSwNP) and shares his expert recommendations on streamlining their recognition and diagnosis, navigating the current unmet needs in patient and clinician education, as well as advocating for strengthened patient support systems. He stresses the importance of healthcare professionals working collaboratively to strategise and exchange best practices. Looking ahead, Gevaert expresses his optimism for the future of care and treatment for patients with CRSwNP.
WHAT IS CHRONIC RHINOSINUSITIS WITH NASAL POLYPS, HOW DOES IT AFFECT PATIENTS’ LIVES, AND HOW IS IT DIAGNOSED?
Chronic rhinosinusitis is a chronic inflammatory condition of the paranasal sinuses and nasal cavities, affecting an estimated 2–12% of the general population.1,2 There are two main phenotypes, based on the presence (CRSwNP) or absence (chronic rhinosinusitis without nasal polyps) of nasal polyps,1 which are bilateral soft tissue growths in the sinuses and nasal cavity.1-3 Individuals with CRSwNP typically have no sense of smell at all, and symptoms such as blocked nose, watery secretions, postnasal drips, as well as cough, facial pain or pressure, can become a constant struggle.1-4 It feels like you are on the third or fourth day of a severe cold, and imagine feeling that way for years. It’s incredibly debilitating, and symptoms negatively impact patients’ lives both emotionally and physically, significantly affecting their quality of life.1,3,5 Sleep is disrupted due to constant nasal blockage, making it hard to breathe.3,4 Your partner might be annoyed because of your constant nasal issues, and at work, it’s hard to concentrate, and due to similarities with the common cold or COVID-19, colleagues may look upon the condition unsympathetically or assume you are contagious. Patients often feel misunderstood because when they tell someone, ‘I have nasal polyps’, the typical response is, ‘Is it bad? Will you die from it?’ The answer is no, you won’t die from it, but you feel horrible and have to live with it, and that is very challenging.
Individuals with CRSwNP frequently have other conditions or comorbidities, and therefore, it is crucial to screen for CRSwNP in patients with asthma, due to the close connection between the two (up to 67% of patients with CRSwNP have asthma).6
“In my experience, pulmonologists are adept at identifying patients with CRSwNP by asking patients with asthma about their sense of smell. This is crucial for all physicians to note, including general practitioners (GP), to ensure prompt diagnosis and comprehensive care for these patients. I recommend that specialists, GPs, and other doctors who experience a patient presenting with asthma and/or long-term symptoms similar to the common cold, ask if the patient can smell. If they can’t, then CRSwNP should be considered.”
COULD YOU DESCRIBE THE PATHOGENESIS OF CHRONIC RHINOSINUSITIS WITH NASAL POLYPS?
“I believe nasal polyps are a backup defence mechanism, growing in the most vulnerable places in the nose and initially serving a protective function. For example, when the body encounters a microorganism it can’t immediately eradicate, it has three options: (1) eradicate it (you win); (2) succumb to it (the microorganism wins), causing sepsis or even death; or (3) build a physical wall, like nasal polyps, where the microorganism stays there (no one wins). There are three main ways our body defends itself, through different types of inflammation: Type 1 (viral infections), Type 2 (parasitic infections), and Type 3 (fungal infections).”
CRSwNP is caused by a dysregulated immune response to foreign agents, triggering mucosal inflammation frequently characterised by a Type 2 inflammatory signature.1,3,6 It’s a complex interplay of genetic and environmental factors that triggers the growth of nasal polyps. Certain individuals are more vulnerable to developing nasal polyps, such as those with immune deficiencies, or inborn or acquired barrier dysfunction.6 Vulnerability may also be acquired after viral infection or due to a range of environmental factors, such as exposure to Staphylococcus aureus, which is present almost everywhere on everything we touch, and may take advantage of an impaired barrier to persist and drive Type 2 inflammation.4,7,8
WHAT ROLE DO TYPE 2 INFLAMMATION AND TYPE 2 CYTOKINES PLAY IN THE DISEASE?
In Europe, around 80–85% of patients with CRSwNP exhibit a Type 2 inflammatory endotype, associated with increased IgE production, elevated local IL-5 levels, and prominent eosinophilic infiltration of tissues.9,10 A heightened Type 2 immune signature is linked with greater disease severity, comorbidities, and disease recurrence after surgical intervention.3,9,10
Type 2 cytokines, such as IL-4, IL-5, and IL-13, play a significant role in driving Type 2 inflammation. Historically, IL-5 was primarily considered the main trigger for eosinophilic inflammation. IL-5 is produced in the tissue and sends a signal through the blood to the bone marrow, where stem cells transform into eosinophils. These eosinophils then travel back through the blood to the tissue where the signal originated.11
“Today, we understand that IL-5 is not only crucial for eosinophils but also contributes to local IgE production and other pathological processes.11 The Type 2 cytokines (IL-4, IL-5, IL-13) are linked, either directly or indirectly, to IgE production, epithelial barrier dysfunction, tissue damage and remodelling, and nasal polyp formation.”(Figure 1)11,12
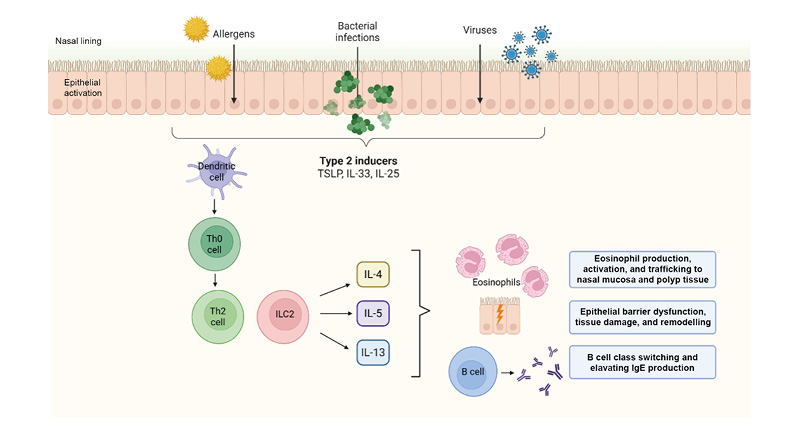
Figure 1: The role of IL-4, IL-5, and IL-13 in Type 2 inflammation in chronic rhinosinusitis with nasal polyps.
Created with Biorender.com.
ILC2: group 2 innate lymphoid cells; Th0: naïve T cell; Th2: T helper 2 cells; TSLP: thymic stromal lymphopoeitin.
HOW CAN EAR, NOSE, AND THROAT SPECIALISTS ASSESS (TYPE 2) INFLAMMATION IN THEIR CLINICAL PRACTICE?
“When I suspect a patient has CRSwNP, my first step is to perform an endoscopic evaluation to identify key signs of inflammation, such as swelling, secretions, crusting, and the presence of nasal polyps.13 To confirm the presence of Type 2 inflammation, we can obtain a nasal tissue biopsy for histopathological analysis (e.g., tissue eosinophils), which can determine whether inflammation is Type 2 or a mix of endotypes. Additionally, nasal secretions can reveal the presence of small dots called Charcot-Leyden crystals, indicative of Type 2 inflammation and contributing to the thickness of mucosal secretions.”14
Blood tests for eosinophils and IgE are also informative to identify Type 2 inflammation, although blood tests are more meaningful when larger organs like the lungs are involved (i.e., a more systemic disease), and may not always be reflective of what is occurring in a smaller organ like the nose. Currently, biopsy or nasal secretion analysis are the best ways of assessing the type of nasal inflammation. Other key indicators that indicate likely Type 2 inflammation in patients with CRSwNP are the comorbidities of asthma, allergic rhinitis, and non-steroidal anti-inflammatory drug-exacerbated respiratory disease.3,10,15,16 The inflammation in the nose and lungs is similar, and I believe that our body likely does not differentiate between the upper and lower airways, and that the two act together as ‘unified airways’, sharing an interconnected inflammatory pattern.
WHAT ARE THE TREATMENT OPTIONS AVAILABLE, AND WHAT CHALLENGES DO PATIENTS FACE IN RECEIVING EFFECTIVE TREATMENT FOR CHRONIC RHINOSINUSITIS WITH NASAL POLYPS?
To treat CRSwNP, nasal saline irrigation and intranasal corticosteroids are recommended, and in more severe cases, short-course oral corticosteroids (OCS) are prescribed.4 However, intranasal sprays are often insufficient for large nasal polyps, as they only reach the tip of the polyps and not the sinuses. Whilst OCS can suppress inflammation and reduce symptoms, their benefits wane shortly after discontinuation, and they come with significant and cumulative side effects, making the cost of treating a patient long-term with OCS very high for society.4,17,18 Long-term or cumulative use is discouraged due to side effects, including diabetes, hypertension, stroke, anxiety, and cardiovascular disease.4,17,18 In patients with severe CRSwNP who are refractory to first-line treatment, surgical intervention should be considered.4,18 Ancient Egyptians and other cultures used snares (looped wires) to remove nasal polyps and rinsed the nose with saline over 4,000 years ago.19 However, simply removing the nasal polyps is like mowing the grass; they tend to come back quickly because CRSwNP is a chronic inflammatory disease of the mucosa.
Therefore, we now perform surgery to remove nasal polyps and the diseased mucosa, opening up the sinuses for better local medication access.4,17,18 Nevertheless, many patients experience recurrence after surgery and may require one or more revision surgeries.3 The recurrence rate of CRSwNP after surgery ranges from 20% to 60% within 18 months to 4 years follow-up, to 79% over a 12-year period (N=38).20 We were able to predict the patients at risk of recurrence and/or revision surgery, such as those with allergies, asthma, aspirin hypersensitivity, and elevated tissue eosinophils/IL-5/IgE; i.e., those with a strong Type 2 inflammation predominance.18,20
After surgery or if a patient is unsuitable for surgery, we consider biologics, which have revolutionised patient care. Three biologic therapies are currently approved in the EU for CRSwNP treatment, including anti-IgE, anti-IL5, and anti-IL-4Rα monoclonal antibodies targeting pathways in Type 2 inflammation.2,21-24 More biologics are on the horizon for CRSwNP, with different targets and longer dosing regimens requiring less frequent injections.24,25 Biologics can decrease symptom severity, nasal polyp size, and the need for OCS and surgery.2,19-26 Moreover, it is vital to initiate biologic treatment in a timely manner in order to prevent severe disease progression, which may involve osteitis or thick bone neoformation. “However, only a minority of our patients receive biologics, and there may also be issues around patient self-administration and adherence, as well as a risk of recurrence if the patient discontinues their biologic.”
“Currently approved biologics can be self-administered subcutaneously and are given every 2–4 weeks.2,22-25 In my clinical experience, a common obstacle to biologic therapies is the fear of self-administered treatment. Patients are afraid of self-injection. They tell me that it hurts, that they are afraid of blood and needles. In my practice, to educate patients and encourage compliance, the first three injections are administered by the nurse within the hospital setting, though this consumes considerable time from the clinicians and nurses.”
It’s also important to inform patients that they need life-long treatments, even though that’s not what they want to hear; they would rather be cured. Furthermore, when the responsibility of regular dosing is placed on the patient, they may become less diligent or compliant over time. Poor adherence may lead to a recurrence of symptoms and inflammation, and prolonged inflammation can increase the risk of complications, like osteitis and disease recurrence. Consistent treatment is essential for long-term management, and treatments that require less frequent dosing could make a huge difference for patients and for us as physicians.
“I have also observed an unmet need in GP awareness around CRSwNP diagnosis and management, resulting in delays in ENT specialist referral and bottlenecks in the patient pathway. Moreover, ENT specialists themselves may be hesitant to prescribe biologics, meaning only a minority of patients will actually receive treatment with biologics. Therefore, early intervention for patients isn’t just about treatment access; it’s about facilitating early referrals to ENT specialists who can perform surgery and/or prescribe biologics. This dual approach will help us to intervene earlier and manage CRSwNP more effectively, and by raising awareness and educating clinicians, we can diagnose and treat patients earlier.”
In addition to the limited awareness amongst diagnosing physicians, there is a lack of patient education regarding CRSwNP. There is a significant need for resources to support patients throughout their treatment journey, to streamline management and alleviate the burden on time-poor healthcare professionals. Fortunately, efforts to create patient resources are already in motion, with the development of the European Forum for Education and Research in Allergy and Airway Diseases (EUFOREA) CRSwNP patient portal, a resource for patients which explores disease information, preparing for consultations, support with diagnosis and treatment, as well as some patient outreach initiatives.27
WHAT EXCITES YOU ABOUT THE EVOLVING TREATMENT LANDSCAPE IN CHRONIC RHINOSINUSITIS WITH NASAL POLYPS?
“In 20 years, I hope we no longer see patients with end-stage disease or with countless revision surgeries due to earlier intervention.” Early surgical intervention has shown to reduce the need for further surgeries and lower the risk of developing severe asthma in patients with CRSwNP. When signs of recurrence appear post-surgery, we need to act quickly. Although data on earlier intervention with biologics for CRSwNP are still emerging, the analogy with asthma treatment suggests that timely biologic therapy may modify the course of the disease and improve patient outcomes in the long run, potentially achieving remission.4 “With the continually advancing growth of biologic therapies and increased possibility of long-term biologic treatment, I believe the future lies in a combined, patient-specific approach of prompt surgery and personalised clinical management. Integrating biologics with surgery could potentially improve surgical and patient outcomes, boost cure rates, and possibly eliminate the need for revision surgeries.”
“The future looks bright. We now understand the disease better, and there are new developments, guidelines, and data in the field almost every week. With growing momentum and awareness in the field, although some unknowns and areas for exploration remain, I encourage clinicians to continue documenting their practices and outcomes, and communicate and collaborate effectively to establish and refine optimal treatment strategies for CRSwNP. We need to share strategies, our experience, and expertise. CRSwNP is now a moving target, and I hope that in future it will no longer be a challenging disease to manage.”
NX-GBL-EOS-WCNT-250001
Date of preparation: August 2025




