Interview Summary
The prevalence of allergic rhinitis (AR) varies between countries but is increasing globally as urbanisation and climate change increase exposure to allergens and irritants such as pollution. For children, schools are a problematic source of allergens and irritants that exacerbate the disease. AR can negatively impact a child’s capacity to attend and perform in school. Appropriate treatment of AR can help to mitigate this impact, but avoidance strategies are also crucial in managing this chronic disease. In select children, allergen immunotherapy may also play an important role. EMJ spoke to three experts in allergy and immunology from China, Portugal, and the USA, who described how and why the prevalence of AR is evolving, and what impacts AR can have on children. They emphasised the importance of early diagnosis and effective treatment for children using standardised treatment guidelines; controlling allergen and irritant exposure in the school environment; and improving the quality of health education among patients, caregivers, school staff, policy makers, and HCPs including paediatricians, general practitioners, and pharmacists, to promote and optimise AR management. They also highlighted the need for strategies to provide allergy-friendly schools to ensure that children with AR can thrive academically, physically, and socially.INTRODUCTION
AR, the most prevalent allergic disease across all age groups, causes a substantial and increasing burden on the health of individuals around the world. Prevalence data suggest that 10.5–19.9% of children globally suffer from AR.1,2 The increasing prevalence and complexity of AR is a consequence of climate change causing increased air temperatures, longer pollen seasons, increased pollen production, and allergenicity of the pollen.3 Increased urbanisation is also driving these changes, exposing children to greater levels of air pollution, which acts as an irritant, increasing their susceptibility to develop AR and exacerbate symptoms.4,5 These environmental changes impact children more significantly compared to adults.6 AR can present in pre-school children as young as 2–3 years old,2 with symptoms including sneezing, itching, nasal congestion, and rhinorrhoea, often misdiagnosed as viral infections.7 Comorbidities such as asthma are common, and estimates suggest that 80% of people with asthma also have AR, while up to 40% of individuals with AR also have asthma.8
School-age children spend significant amounts of time in educational settings. Many schools have inadequate ventilation and ageing infrastructure that can increase the presence of allergens and contribute to poor health among staff and students, increasing absenteeism, presenteeism, and impacting academic performance.9 Even modern school buildings can increase allergen and irritant levels, when natural ventilation is reduced to help increase energy efficiency. In heavily polluted cities, air pollutants can enter the classroom, including sulphur dioxide (SO2), and particulate matter (PM) 2.5 and PM10, at levels higher than recommended by the WHO. Exposure to these pollutants can exacerbate respiratory symptoms,10-13 and perpetuate educational inequalities in settings where school revenues are linked to student attendance rates.14
AR can have far-reaching effects on a child’s quality of life, mental health, and academic performance.6 Poorly controlled AR has been shown to result in lower academic productivity due to AR symptoms, use of sedating antihistamines, poor sleep quality, and increased absenteeism.15,16 Studies show that children with allergic conditions are more likely to be in a lower quartile for reading ability,17 and can be at increased risk of bullying and victimisation compared to children without respiratory conditions.18,19 Achieving good AR and asthma control can return school performance to normal.20
Current treatment recommendations for paediatric AR are based on the frequency of symptoms and the impact on the quality of life.21 In the Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines,22 symptoms experienced less than 4 days a week or less than 4 consecutive weeks are considered intermittent, whereas in persistent AR, symptoms last more than 4 days a week and 4 consecutive weeks.23 AR severity is categorised as mild when there is no impact on daily activities or sleep, or moderate-to-severe when symptoms interfere with sleep, daily activities, or school, or trigger serious sequelae like asthma attacks (Table 1).24
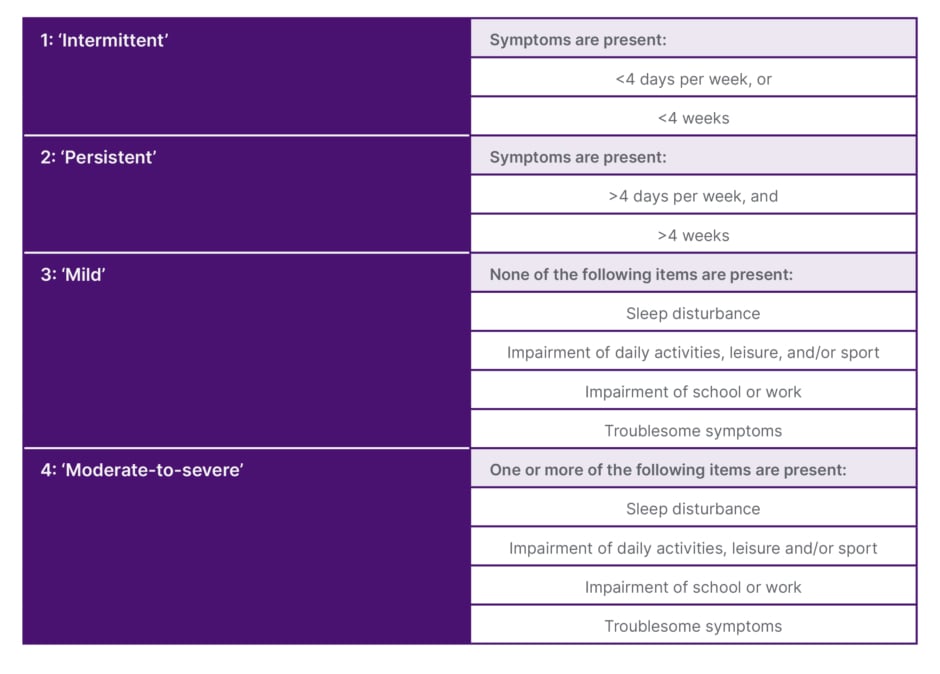
Table 1: Classification of allergic rhinitis.24
To understand how the management of AR can be improved to reduce the burden of disease on children, particularly in the school environment, EMJ spoke to three allergy experts: Michael Blaiss, Clinical Professor of Paediatrics, Medical College of Georgia, Augusta Georgia, USA, and Past President of the American College of Allergy, Asthma, and Immunology (ACAAI); Lei Cheng, Professor of Otorhinolaryngology & Director of Clinical Allergy Center, The First Affiliated Hospital with Nanjing Medical University, China, and current President of the Chinese Society of Allergy; and Mário Morais-Almeida, Head of Allergy Center, CUF-Descobertas Hospital, Lisbon, Portugal, and current President of the World Allergy Organization (WAO). The experts’ wide-ranging insights into the impact of AR on children highlight the need for better education among stakeholders to ensure best practices are understood, shared, and implemented consistently around the world. In addition, the experts agreed that existing policies to create allergy-friendly schools should be more widely adopted to reduce health inequalities and allow every child to thrive both in, and outside of, the classroom.
EVOLVING ALLERGIC RHINITIS PREVALENCE, SEVERITY, AND COMORBIDITIES
The number of children experiencing AR is increasing across the globe. “In China, we have observed a rapid increase in both population-based surveys and hospital-based diagnosis data in the past decades. People affected by self-reported AR increased by almost 100 million in 2011 compared to 2005,” Cheng explained. A meta-analysis of Chinese epidemiological studies of children found that the diagnosed prevalence of allergic rhinitis from 2012–2021 was higher (19.75%) than that from 2001–2011 (14.81%).2,25 “These are astonishing figures,” Cheng said, explaining that increasing urbanisation, pet ownership, and air pollution are driving the AR epidemic. Blaiss and Morais-Almeida agreed, adding that, in the USA and Europe, AR prevalence has reached up to 40%, with children increasingly affected, and comorbidities including asthma, eczema, chronic rhinosinusitis, and sleep-disordered breathing increasing too, particularly in urban areas.4
Morais-Almeida stated that, in his experience, more young children (3–5 years old) are presenting with chronic rhinitis,26 and about 25% of them with moderate-to-severe symptoms, although not all in the allergic form. In addition, Morais-Almeida explained that many people in Portugal and other parts of southern Europe are experiencing persistent AR. This is most likely because of the effects of climate change, which is lengthening pollen seasons and increasing air pollution. Cheng outlined how, in China, the predominant allergens vary according to region. In Southern regions of China, dust mites are the leading cause of AR, whereas plant allergens, including mugwort, ragweed, and dandelion, are the most common allergens in the Northwest of the country. In urban areas, afforestation with anemophilous plants can cause seasonal allergies in the spring. This contrasts with summer and autumn allergies that are mostly caused by weed pollen from species including Atermisia spp., Hummulus spp., and Chenopodium quinoa, Cheng added. Blaiss concurred and said that outdoor allergens in the USA also vary depending on region. “Knowing the particular allergens in your area and time of pollination is important in limiting outdoor exposure,” Blaiss added.
Data from the International Study of Asthma and Allergies in Childhood (ISAAC) has shown that AR often begins in early life, with prevalence increasing with age.27 The experts noted that comorbidities such as asthma are increasingly common. “This is concerning because, apart from genetics, AR is the main risk factor for asthma in early life,”28,29 Morais-Almeida emphasised. “We need to treat AR effectively as early as possible to prevent progression to asthma.” In the USA, in 2021, 18.9% of children experienced seasonal allergies,30 Blaiss explained, adding that severity appears to be increasing too, with a recent study suggesting that air-conditioned environments may increase disease severity in children.31
DEVELOPMENT OF EFFECTIVE AR TREATMENT GUIDELINES
Evidence-based guidelines for the treatment of AR are being implemented across the globe. In Europe and the USA, the ARIA guidelines7,21 form the basis for the treatment of mild and moderate-to-severe, intermittent, or persistent AR. In China, guidelines were first developed in the 1990s by the Chinese Medical Association and allergy experts, with regular updates every 6–7 years.3 According to Cheng, the publication of the ARIA guidelines in 2001 had an important impact on the Chinese guidelines.32 Now, the Chinese guidelines, informed by research in China and internationally, align closely with the ARIA guidelines, recommending four types of drugs as first-line treatments for AR, including oral second-generation antihistamines, nasal glucocorticoids, nasal antihistamines, and leukotriene receptor antagonists (LTRA).25 “Our guidelines focus on continuous improvement, which has led us to a system with Chinese characteristics that incorporates international experience to improve diagnosis and treatments,” explained Cheng. In 2022, the updates included separate guidelines for adults and children that are very specific and easy for HCPs to follow. Cheng also outlined that the Chinese guidelines follow the principle of combining prevention and treatment, with a ‘four in one’ approach: environmental control, pharmacotherapy, immunotherapy, and health education.33 In the Chinese guidelines, first-line drug monotherapy is usually effective in mild, intermittent AR. For moderate-to-severe, persistent AR, a combination of a nasal glucocorticoid and a second-generation antihistamine and/or LTRA, is recommended.33 Allergen-specific immunotherapy (AIT) is also recommended as first-line treatment for AR in Chinese guidelines.33
CHALLENGES OF IMPLEMENTING GUIDELINES: TRIVIALISATION OF ALLERGIC RHINITIS AND RISE OF MISINFORMATION
Despite the availability of evidence-based guidelines for the management of AR, in many cases, AR is not managed effectively. The experts agreed that paediatric AR is too often trivialised by caregivers and HCPs, and outlined some challenges encountered with implementing the guidelines in practice. AR symptoms may start with an itchy nose and sneezing, but can develop to nasal obstruction, persistent cough, and sleep disruption. Morais-Almeida explained that, often, when patients go to the doctors to talk about their AR symptoms, they end up focusing on other conditions or symptoms, such as experiencing a high number of respiratory infections, restless sleep, snoring, and headaches. The HCPs may also feel that some symptoms are more important to discuss, and the AR may not be considered fully. “Several of these manifestations that came to the ‘podium’ at the consultation are common complications or comorbidities of an under-recognised and under-treated allergic rhinitis,” Morais-Almeida emphasised.
However, many people self-medicate for AR with over-the-counter medications without consulting with an HCP. Blaiss is worried that misinformation circulating on social media is exacerbating non-compliance and creating fear among patients. “In the USA, we are increasingly seeing non-compliance to medication among patients, and lack of understanding of how to use medication. For example, parents may delay taking their child to see a paediatric allergist due to their belief in online testimonials claiming AR can be managed ‘without doctors’ or ‘cured naturally’.” Also, according to Blaiss, many people with AR are unaware that they need to medicate before symptoms worsen. “Patients and caregivers need to understand that individuals with AR will maintain better symptom control if they start medication before symptoms build up, rather than waiting until symptoms become severe, and that they should be taking medication regularly,” Blaiss explained.
Another issue, Morais-Almeida said, is that people buy medication from pharmacies that are sold in small boxes, which can create issues for compliance and consequently for control. Patients could benefit from an AR management plan, with clear recommendations on treatment duration. Another concern, said Blaiss, is that people are increasingly using homeopathic remedies, advertised on social media, for which there is no scientific evidence on efficacy or safety.
OPTIMISING TREATMENTS FOR PAEDIATRIC PATIENTS WITH ALLERGIC RHINITIS
To standardise treatment in paediatric patients with AR in the USA and Europe, the EUFOREA algorithm for treatment escalation and de-escalation in children is closely followed.7 First-line care for mild intermittent or persistent, and moderate-to-severe intermittent AR includes second-generation antihistamines, and addition or replacement with nasal corticosteroids when symptoms are not controlled.7 In China, there are specific AR guidelines for children, with detailed recommendations on pharmacotherapy.33 Cheng emphasised the need to use second-generation antihistamines to minimise sedation and other cognitive adverse events. “For the treatment of AR in children, non-sedating second-generation antihistamines are recommended to avoid central nervous system inhibition that may affect cognitive function,” Cheng said. He continued: “In patients with moderate-to-severe and persistent AR, we would recommend combining second-generation antihistamines with intranasal corticosteroids that have low systemic bioavailability because it is important to ensure growth is not affected, especially when some children with persistent AR require corticosteroids for 12 weeks or more.” It is also very important that clinicians pay particular attention to age limits for medications, choose appropriate doses, and consider potential adverse drug reactions. “Every doctor should know that children are not mini versions of adults,” Cheng emphasised.
The challenges of optimising treatment for paediatric AR are not limited to HCP recommendations, as many caregivers choose to treat without consulting with an HCP, which the experts believe can sometimes lead to either suboptimal treatment selection or incorrect administration. All three experts highlighted the importance of the role of the HCP to ensure prompt and effective control of AR in children to avoid progression to more severe symptoms and comorbidities, in particular asthma. Morais-Almeida summarised the point saying: “It is important to control AR today and next week, to reduce the impact on everyday activities and school performance, but it is also important to treat for the future.” If pharmacotherapy is not sufficient to improve quality of life and sleep to an acceptable level, the individual should be referred to a specialist and allergen-specific immunotherapy (AIT) may be appropriate, Blaiss added.
Encouraging shared decision-making between children, caregivers, and HCPs is also crucial for successful management of AR, the experts said. Morais-Almeida recommends starting conversations with young patients as early as possible. Blaiss agreed, saying: “When you have the patient and their caregiver in the room, you need to explain the treatment options, and work with them to decide what they find most acceptable. For example, there is no point in prescribing an intranasal corticosteroid if they say they won’t use a nasal spray. The patient is a partner, and you need to agree on what treatment regimen will best suit the patient’s lifestyle.”
IMPACT OF THE SCHOOL ENVIRONMENT ON PAEDIATRIC ALLERGIC RHINITIS
Most children spend many of their waking hours at school, an environment that can trigger allergies. Allergens in schools range from dust mites in carpeting, bookshelves, and toys, to animal dander on classmates’ clothes, and mould and cockroaches in poorly maintained buildings. Allergy symptoms can be further exacerbated by irritants from cleaning products and air pollutants due to insufficient ventilation systems. As Blaiss explained, children and adolescents spend much of their time either in their bedroom or the classroom, and while the home environment can be adapted to reduce allergen exposure, the school environment is more difficult for the individual or caregiver to control.
The impacts of uncontrolled AR on children are significant. Sleep disruption, sneezing, and rhino-conjunctivitis make it difficult for children to concentrate and function as normal during the day. Children who experience AR symptoms, or need to take medication at school, also often have feelings of social isolation and self-consciousness.16 Blaiss highlighted studies showing that AR and allergic rhino-conjunctivitis (ARC) can affect academic performance, with students performing less well in summer exams than similar level tests taken during the winter months.16 A questionnaire-based study of academic productivity in people aged 13–29 years also demonstrated the negative impacts of AR.15 The findings of these studies emphasise the importance of ensuring that clinicians gain a better understanding of the unique burden that AR places on children. Ensuring HCPs, school staff, and caregivers understand the impact of AR on children would help them to receive prompt and appropriate treatment to improve both clinical and academic outcomes. Blaiss and Morais-Almeida noted that, in the USA and Europe, there is limited education in medical schools on AR, and, in the USA, no mandatory training for resident doctors in allergy and immunology. Increasing education about allergies for new doctors can enable them to make better informed recommendations on AR management, particularly by avoiding medications that impair concentration, like first-generation antihistamines. The experts agreed that better education for HCPs, caregivers, and patients would improve awareness of AR and its triggers, help to reduce the detrimental impact of AR symptoms and suboptimal medication, and support better quality of life and academic performance for young people.
STRATEGIES TO REDUCE THE IMPACT OF ALLERGIC RHINITIS ON SCHOOL CHILDREN
Environmental Control
Environmental control strategies can help reduce exposure to allergens and irritants. Cheng reiterated that many children’s AR symptoms can be significantly improved through environmental control measures, which is one of the four priority areas for primary intervention outlined in the most recent Chinese AR treatment guidelines.25,33 Some urban schools in China are reducing air pollution and pollen concentration in classrooms and trying to avoid stimuli, like cold and heat alternation, that can exacerbate allergic symptoms, Cheng said.
The experts agreed that more should be done to help reduce exposure to allergens in the school environment. Conditions vary hugely between regions and between individual schools in the same region; however, the experts identified adaptations that help, including removal of soft furnishings and carpets, regular maintenance of air filtration systems, use of allergy-friendly cleaning products, and limiting pets in the classroom. Children with pollen allergies could be allowed to stay indoors during break times when pollen forecasts are high.
Health Education
In China, the most recent AR guidelines introduce advice on prevention measures, and in the children’s guidelines emphasise the value of health education to improve disease awareness, avoidance of allergens through environmental control, and treatment compliance.33 Following recommendations from the WAO to standardise treatment and management through the education of HCPs, the Chinese Society of Allergy developed a programme of talks to encourage utilisation of guidelines through continuing medical education (CME). “At the same time, by combining doctor education and patient education, we are vigorously promoting medical science popularisation projects,” Cheng said. He went on to explain that there are two benefits to this: “The first is to increase awareness of AR and to increase compliance of treatment. The second benefit is that HCPs are better equipped to make accurate diagnosis and standardise treatment, adhering closely to published guidelines and thereby improving the quality of AR management.”
An important element of health education, said Blaiss and Morais-Almeida, is to advise patients and caregivers on the sedative effects of first-generation antihistamines. Portugal has approximately 10 million inhabitants and, according to Morais-Almeida, each year, approximately one million packs of first-generation antihistamines are dispensed from community pharmacies, many of them as over-the-counter medicines without prescription. “These medicines cause drowsiness and have other potentially harmful side-effects in a significant percentage of our population, including in the paediatric age group,” Morais-Almeida explained. “This is problematic for children, impacting their ability to concentrate in school, and for adults where, for example, the sedation impairs driving performance and psychomotor function, including reaction time.34 Both Blaiss and Morais-Almeida noted first-generation antihistamines no longer have a place in AR treatment, and are not recommended in any AR treatment guidelines, a view that is widely supported by a recent publication in the WAO journal, and others.35,36
Public Engagement
Projects to engage and educate physicians, pharmacists, and the general public on AR management are helping to raise awareness of AR and strategies to reduce exposure and achieve more effective symptom control. ‘’We have a project in Portugal called ‘News about pollen’ which is a weekly TV show that started 18 years ago to empower people with information about allergens, pollution, and the impact of allergic diseases, including AR, asthma, and atopic dermatitis,” explained Morais-Almeida. “This helps us to empower the population to choose medications wisely, and at the same time to involve HCPs and pharmacists. We highlight the right way of using the treatments and promote non-sedating medications.”
The Control of Allergic Rhinitis and Asthma Test (CARAT) is a tool to assess control of AR and asthma in adults and children37-39 that was developed in Portugal and promoted and used widely. CARAT has been translated into more than fifteen languages and is used in countries around the world, being recommended by ARIA, Morais-Almeida explained. “This is important because it is very difficult to get control of asthma if you don’t get control of AR.” New digital tools are also helping to empower patients to take control of their condition in terms of symptom management, allergen avoidance, and treatment.40-42
In China, public lectures and academic forums are used to engage with the public to increase awareness of AR and encourage early diagnosis, treatment, and prevention, to avoid exacerbation, recurrence of symptoms, and exposure to new allergens. Cheng highlighted the WAO’s World Allergy Week43 as an important event that is helpful to raise awareness of AR with public audiences. “For children and adolescents with AR, education can improve the relevant knowledge level and treatment compliance of patients, help reduce the recurrence rate and complications of AR, and improve patient quality of life by alleviating their physical and psychological symptoms,” Cheng reiterated.
Promoting Allergy-Friendly Schools
The experts believe that teachers and school staff need to be better informed about the impact AR can have on their students, and what mitigation strategies can be put in place. Environmental control measures are important to reduce allergen exposure in school, including the choice of trees planted in the grounds and procedures for cleaning classrooms. “Often classrooms are cleaned and then closed at the end of the day without any ventilation, exposing children to irritants the following morning,” said Morais-Almeida. “We need to focus on air quality.”
Blaiss and Morais-Almeida believe that AR management plans developed in collaboration with caregivers and doctors, similar to the mandatory asthma action plans, would help children with AR to navigate the school environment and empower teachers to support individuals’ needs. Cheng agreed, saying: “Children spend a lot of time at school, so the school environment is one that we need to control.” In China, efforts are being made to encourage allergy-friendly educational environments, from nurseries to middle schools and beyond, but more can be done in less developed areas to make changes to become more allergy-friendly. “Our goal is to provide allergy-free schools,” Cheng said, which he believes should be the optimal goal when talking about holistic paediatric AR management.
CONCLUSION
The impact of AR on children and their ability to thrive in and out of the classroom should not be underestimated. More needs to be done to optimise diagnosis, treatment, and education to enable and encourage schools to create environments that are free from allergens, so that all children can thrive academically, physically, and socially. Raising awareness of best practices in the management of AR, including shared decision-making between patients, caregivers, and HCPs, is vital to improve adherence, quality of life, and treatment outcomes.




