Meeting Summary
Hereditary angioedema (HAE) is a rare genetic condition that causes unpredictable, recurrent episodes of swelling, particularly affecting the limbs, face, gastrointestinal tract, and airways. Episodes can be debilitating or even life-threatening if not managed properly. Beyond the physical burden, HAE profoundly impacts quality of life, leading to pain, anxiety, and significant social and occupational limitations. Many patients face constant fear of the next attack and feelings of isolation. Treatment guidelines focus on normalising patients’ lives by controlling symptoms and reducing attack frequency and severity, aiming to help patients fully participate in daily activities without fear. A BioCryst-sponsored symposium took place at the 14ᵗʰ C1-inhibitor Deficiency and Angioedema Workshop in Budapest, Hungary. The symposium was chaired by Henriette Farkas, Professor of Internal Medicine and Director of the Hungarian Angioedema Reference Center, Department of Internal Medicine, Semmelweis University, Budapest, Hungary. The panellists discussed what the goal of normalisation of patients’ lives means in real-world practice. Marc Riedl, Professor of Medicine, Division of Allergy and Immunology, University of California, San Diego, USA, spoke on the burden of illness of HAE, exploring unmet needs and the importance of a comprehensive assessment to enhance care for adults with HAE. Andrea Zanichelli, Head of Angioedema Centre, IRCCS Policlinico San Donato, Milan, Italy, explored key considerations for switching HAE treatments in adults to optimise outcomes. Tamar Kinaciyan, Head of Allergy and Paediatric Dermatology Clinics, Department of Dermatology, Medical University of Vienna, Austria, discussed practical considerations for individualised HAE management approaches in adolescents to support life normalisation.
Introduction
The symposium opened with a powerful reminder of why patient-centred care must remain at the heart of HAE management. Farkas shared a patient perspective, exploring the emotional and physical toll of living with HAE, ranging from disfiguration and pain to feelings of isolation, fear, and sadness. Through patient-created artwork, the audience was given a unique insight into the lived experience of HAE, emphasising the profound impact beyond clinical symptoms. Farkas noted that “these patients inspire us to help”, setting the tone for a session focused on recognising the burden of illness, addressing unmet needs, and advancing individualised treatment strategies, including in adolescence, to help patients reclaim a sense of normality.
Introduction to Hereditary Angioedema
HAE is a rare genetic disorder characterised by unpredictable, recurrent episodes of angioedema affecting subcutaneous or mucosal tissues.1 HAE attacks typically involve the skin, gastrointestinal tract, and upper respiratory tract.1 Attacks affecting the upper airways are particularly dangerous due to the risk of sudden airway obstruction and asphyxiation.1 Without treatment, these attacks can gradually intensify over a period of 12–36 hours before resolving spontaneously within 2–5 days.2 On average, untreated patients experience an attack every 2 weeks, with frequencies ranging from very rare to every 3 days.1,2 The two primary types of HAE result from mutations in the SERPING1 gene, leading to either a quantitative deficiency (Type 1) or a functional impairment (Type 2) of the C1-esterase inhibitor (C1-INH).1 C1-INH acts on multiple pathways, including the fibrinolysis and coagulation, kallikrein-kinin, and complement systems.3 Dysregulation of these pathways, particularly the kallikrein-kinin system, leads to excessive bradykinin production, which is the primary mediator of the vascular permeability and oedema seen in HAE attacks.4 A third, less common form of HAE exhibits a comparable clinical phenotype, but with normal levels and function of the C1-esterase inhibitor protein (HAE with normal C1INH [HAE-nC1INH])3 Patients still experience similar recurrent angioedema attacks, suggesting the involvement of other genetic factors, such as mutations in the F12 gene (encoding factor XII), plasminogen, or angiopoietin-1.3
Hereditary Angioedema Treatment
At the 14th C1-inhibitor Deficiency and Angioedema Workshop in Budapest, Hungary, both Riedl and Zanichelli discussed the current treatment guidelines for HAE, the goal of which is to normalise patients’ lives by achieving full symptom control and reducing the frequency and severity of attacks, ultimately enabling individuals to participate in daily activities without fear.5 There is a vital role for on-demand treatment in HAE. The WAO/EAACI 2021 guidelines for managing Type 1 and 2 HAE recommend that all patients have immediate access to acute, on-demand medication, and that on-demand treatment is used to treat all attacks as early as possible.5 Zanichelli explained that, in addition to on-demand treatment, long-term prophylactic treatment (LTP) is needed to achieve the goals of total disease control and life normalisation.5 He stressed that the need for LTP should be reassessed at every patient visit, considering disease activity, disease burden, level of control, and patient preferences. He added that “an action plan should be updated at every visit”, in line with guideline recommendations that patients receiving LTP should be routinely monitored to evaluate disease activity and treatment effectiveness, ensuring ongoing optimisation of therapy and outcomes.⁵
LTPs are treatments designed to prevent attacks in patients with HAE. These therapies work by targeting different steps in the disease’s underlying mechanisms. Prophylactic therapies currently recommended by WAO/EAACI include intravenous plasma-derived C1-INH, subcutaneous anti-kallikrein monoclonal antibodies, and kallikrein inhibitors.5 By intervening in these pathways, LTPs help reduce the frequency and severity of HAE attacks, offering patients greater control over their symptoms and improved quality of life (QoL). Attenuated androgens, such as danazol, were historically used for LTP of HAE.5,6 However, due to their unfavourable side effect profile, current clinical guidelines recommend their use only as a second-line option.5
The Burden of Hereditary Angioedema Beyond Attacks
Riedl described the timeline for a patient with HAE as one marked by intermittent, unpredictable attacks, followed by persistent QoL disruptions in the periods between these attacks,2 illustrated in Figure 1. The direct burden of each attack is determined by the location of the swelling, the severity and duration of symptoms, the need for hospitalisation, and the disruption of daily life caused by the attack itself.2 However, Riedl also noted that “HAE is much more complicated than just the swelling episodes that we see in our clinic,” highlighting the broader impact of the disease on patients’ lives.
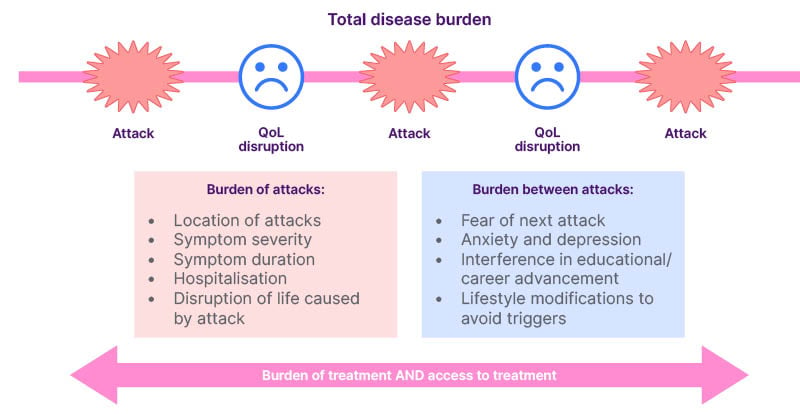
Figure 1: The total disease burden of hereditary angioedema.
Figure adapted from Bork et al2. QoL: quality of life.
The overall disease burden extends beyond the severity of individual attacks, encompassing the psychological and social challenges of living with an unpredictable, potentially life-threatening condition.2 Riedl commented that even during asymptomatic periods, patients often report a constant fear of the next attack, which leads to heightened anxiety, depression, and a sense of uncertainty.2 This anticipatory anxiety can interfere with education, career development, and social interactions, which worsens with increasing frequency of attacks.7 In an effort to prevent attacks, patients frequently modify their lifestyle to avoid known triggers, which can lead to feelings of isolation and a loss of normalcy,2 with Riedl commenting that patients with HAE often experience depression and anxiety.7
Riedl described a non-interventional survey of 445 patients with HAE in the USA, which explored patients’ perspectives on the burden of HAE.7 Health-related QoL worsened with increasing frequency of HAE attacks. However, scores for the “concern about offspring” dimension remained consistent across all attack frequency categories, indicating that this worry is independent of how often attacks occur. Further to this, Riedl highlighted that even a low frequency of attacks was enough to erode the ability to work and participate in regular activities.
Further supporting these findings, a cross-sectional survey of 242 patients with HAE Type 1 or 2 in Australia, Austria, Canada, France, Germany, Spain, Switzerland, and the UK8 revealed that QoL scores worsened with a higher number of attacks. Moderate-to-severe anxiety was reported by 38% of patients, and depression by 17%. The severity of anxiety and depression was closely associated with poorer QoL and reduced productivity. Of note, attack frequency did not appear to influence the severity of anxiety or depression, nor did it affect scores in the ‘fear and shame’ domain. Riedl commented that how patients feel about living with HAE does not necessarily reflect how frequently they experience attacks and that, for many people, “the fear and unpredictability is always there”.
Treatment-Related Burdens in Hereditary Angioedema
Riedl explained that patients also suffer treatment-related burdens, such as anxiety around needing to take their medication. He cited a survey that revealed significant emotional burden, with patients feeling nervous (47%), overwhelmed (33%), stressed (31%), and intimidated (26%) when starting a new prophylactic medication.9 Riedl explained: “People do adapt after being on a treatment for a while, but the burden doesn’t go away.” In the study, anxiety was found to be reduced, but not eliminated in patients who started prophylaxis ≥7 months ago (42%) compared to patients who had started prophylaxis in the previous 6 months (71%).9 Riedl noted that these persistent psychological burdens are a key driver for ongoing innovation in HAE treatments, underscoring the need to develop less burdensome ways to control the condition.
A Comprehensive Approach to Care
Patients and physicians are generally aligned in their selection of prophylactic therapy, as demonstrated by a survey of 109 HAE physicians and 75 patients with HAE-C1INH Type 1 or 2, which explored prescribing trends and the impact of treatment on patients.10 Illustrated in Figure 2, patients placed slightly more importance than physicians on self-administration (77% versus [vs] 65%), while physicians were more concerned with effectiveness (85% vs 81%), side effects (72% vs 57%), and injection site discomfort (60% vs 46%).10 Riedl highlighted that, although patients and practitioners are relatively well aligned, there is a need to understand each patient’s needs and goals on a personal level. He commented: “There is a lot of science to what we do, but also this art of talking to our patients, learning what’s important to them, and helping them make management decisions.”
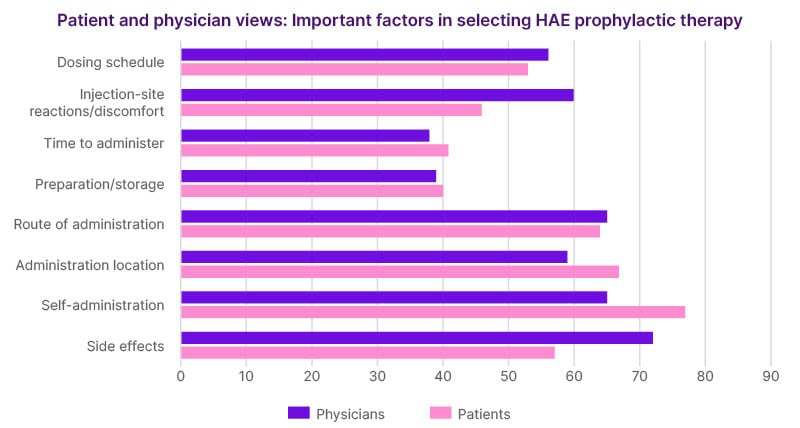
Figure 2: Hereditary angioedema quick guide.
HAE: hereditary angioedema.
To explore and understand patient goals, Riedl introduced the 3D Model of Shared Decision-Making in HAE, originally proposed by Banerji et al.11 This cyclical process comprises three stages: DISCOVER, where clinicians and patients explore patient needs, establish goals, and acknowledge the availability of treatment options; DISCUSS, which involves reviewing alternative treatments, ensuring alignment with patient goals, and developing informed preferences; and DECIDE, where shared decisions are made based on accurate information, guided by validated patient-reported outcome measures. Riedl emphasised that it is the clinician’s role to offer expert insight into what different treatments involve, enabling patients to make informed choices. He also highlighted that treatment decisions are not a one-time event, but part of an ongoing process in which the care plan is revisited and adjusted as needed.
Many patients with HAE don’t feel in control of their condition, leading them to avoid certain activities, with a knock-on impact on their QoL.4 Riedl commented: “I am always surprised at what my patients are telling me. They may not be travelling, they may be skipping family activities, not exercising.” This highlights the need to rethink how clinicians approach conversations about HAE management. Rather than starting with broad, open-ended questions like “How are you doing?” or “Tell me about your symptoms,” Riedl advocated for more specific, targeted inquiries that directly address the patient’s experience of living with HAE (Figure 3).
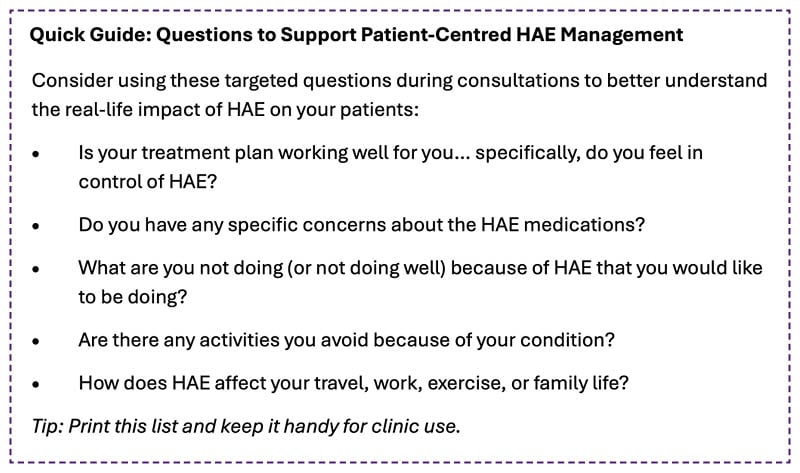
Figure 3: Hereditary angioedema quick guide.
HAE: hereditary angioedema.
Refocusing the conversation in this way helps uncover unmet needs and guides meaningful, patient-centred care.
Optimising Outcomes: Switching Treatments in Hereditary Angioedema
LTP has been shown to significantly reduce the burden of HAE compared to on-demand therapy, enabling better disease control and improved QoL. Presenting results from Zarnowski et al.12 investigating outcomes in 37 HAE patients in Germany, Zanichelli explained that LTP in HAE was associated with reduced anxiety and depression. In the same study, anxiety was significantly associated with low disease control measured by the Angioedema Control Test (AECT),11 further demonstrating the need for control of HAE attacks as a means of achieving life normalisation and reducing burden of disease.
Current recommended first-line LTP options that target C1-INH or kallikrein, have shown benefits but many patients continue to rely on second-line LTP therapy with androgens such as danazol.5 Zanichelli explained that use of androgens is associated with a broad range of adverse effects. These include mood disturbances, such as depression and anxiety, headaches, acne, voice changes, hypertension, liver function abnormalities, lipid profile changes, polycythaemia, changes in libido, weight gain, and muscle pain or cramps.5,10,13,14 In female patients, additional risks include virilisation effects such as hirsutism, deepening of the voice, reduced breast size, and menstrual irregularities, as well as potential risks to foetal development.5,10,12,13 In adolescents, there are concerns about the impact of androgens on bone development and the potential for premature puberty.13
Androgen use has also been linked to increased rates of comorbidities in adults with HAE.15 Zanichelli presented data from a retrospective cohort study involving 446 adults with Type 1 or 2 HAE who were referred to Milan and Padua angioedema centres between 1979 and 2021.15 The study found that patients on androgen-based LTP (n=175) had a significantly higher incidence of comorbidities, including hypertension, hypercholesterolaemia, diabetes, hepatic angioma, and focal nodular hyperplasia compared to those not receiving androgens.15
Guidelines recommend prescribing androgens only as second-line LTP at the minimum effective dosage, up to 200 mg/day, to limit adverse outcomes;5 however, efficacy has been shown to decline substantially at lower dosages. Zanichelli presented data from a retrospective case series that examined danazol use as LTP in 74 patients with Type I or II HAE.16 Danazol was initiated at 600 mg/day, with the dose tapered in patients who achieved complete control. While 96% of patients (n=71/74) achieved complete control at 600 mg/day, this rate fell to 80% at 400 mg/day (n=57/71), and 28% (n=16/57) at 200 mg/day. These findings underscore the clinical dilemma explored by Zanichelli: while dose reduction is necessary to minimise harm, doing so may significantly compromise disease control. This reinforces the need for patients to utilise alternative therapies that offer both efficacy and improved safety.
Androgen Discontinuation and Switch Management
Discontinuing androgens in patients with HAE requires careful consideration, as abrupt cessation is not recommended and should be avoided where possible.5,13,17 Discontinuation due to adverse events is relatively common and has been associated with withdrawal symptoms, including mood disturbances such as anxiety, depression, and irritability, fatigue, and elevations in liver transaminases.13,17 Additionally, stopping androgen therapy may result in an increased frequency and severity of HAE attacks.13 Despite these risks, there is currently no consensus on optimal switching strategies to alternative LTP therapies and guidelines highlight the need for further studies to inform best practices for discontinuation and transition to newer agents.5 Zanichelli outlined possible approaches (illustrated in Figure 4), including tapering androgens with or without a washout period. He highlighted that, ideally, tapering should begin only after the initiation of an alternative LTP agent, particularly when the new therapy requires time to reach steady-state concentrations or its minimum effective dose.17 This strategy reduces the risk of breakthrough attacks during the transition, although patients should be prepared for attacks, with on-demand therapy that they feel confident in administering.13 Zanichelli advocated for switching protocols to be individualised based on the patient’s current androgen dose, clinical status, and risk profile,13 and emphasised the importance of regular monitoring post-switch to assess both efficacy and safety, and support with adherence during the transition period.
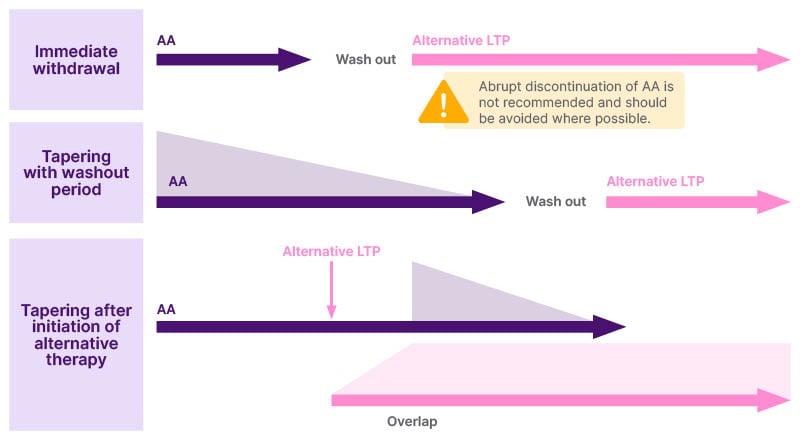
Figure 4: Potential strategies for androgen discontinuation in hereditary angioedema.
There is currently no clear consensus within WHO/EACCI guidelines for discontinuation strategy; however, immediate withdrawal should be avoided.5,13,17 Options for discontinuation include tapering with or without a washout period.13,17 Zanichelli commented that tapering without a washout period, providing a direct overlap, may be important if alternative therapy takes time to reach steady state or minimum effective concentration.
AA: attenuated androgens; LTP: long-term prophylaxis.
Optimising Outcomes in Adolescent Hereditary Angioedema
In the final presentation in the symposium, Kinaciyan explored the impacts of HAE on adolescents, including practical considerations for optimising their care.
HAE can have a particularly profound impact on adolescents, who find themselves in a unique and challenging stage of life.18 Kinaciyan discussed that they are no longer children, yet not quite adults, striving for independence while still relying on adult guidance, with limitations that are made even more pronounced by their illness. Kinaciyan commented that many adolescents with HAE feel embarrassed or ashamed about their condition, struggle to keep up with friends, and may be reluctant to carry or use their acute treatments, often delaying them until absolutely necessary. Further, she discussed how adolescents typically prioritise spending time with friends and mimicking their behaviour, including smoking, drinking, and late-night activities like dancing, all of which can trigger attacks, leading to more frequent or severe episodes. Adolescents may also experience more fatigue than younger children and react more strongly to stress, sometimes becoming aggressive, withdrawn, or depressed.18 Kinaciyan explained: “If the (adolescent) patient is suffering from HAE, you can imagine it is more difficult, and they are limited by their illness.” For these reasons, it is crucial to support adolescents with HAE in living as close to an attack-free, normal life as possible.
Beyond Symptoms: Comprehensive Care for Adolescents with Hereditary Angioedema
Kinaciyan explained that HAE treatment plans for adolescents may differ from those for adults due to the unique life decisions they face, such as choices around education, career aspirations, and family planning. She emphasised that “Understanding individual treatment preferences and goals through shared decision-making is very important.” To support this, a detailed and collaborative discussion should be held when developing an individualised treatment plan.5 Throughout this process, the evolving role of parents as adolescents mature should also be carefully considered. Based on her own experience, Kinaciyan suggested that for patients aged 12–14 years, parents should be involved in discussions to facilitate informed decision making, but for those aged 15–18 years, adolescents should have independent discussions with healthcare providers, explaining that “They can say their real needs more openly if the parents are not by their side”. She commented that these conversations should explore the adolescent’s interests, talents, and aspirations, as well as their treatment preferences and goals. Kinaciyan also noted that it is also important to explain the distinction between on-demand treatment and LTP. Key treatment goals for adolescents include the treatment having few side effects, being highly effective, and allowing patients to be able to participate in all activities.18 Kinaciyan explained that LTP is often the most suitable treatment approach to achieve this. However, she commented that an oral route would allow for easier administration, offering a less cumbersome treatment option without the need for injections.
Practical Considerations of Hereditary Angioedema in Adolescents
LTP recommendations for adolescents largely mirror those for adults; however, the dosing interval and dose is often adjusted considering individual response and body weight.5 Wherever possible, androgens should be avoided due to their potential interference with growth and maturation processes.5 As with adults, individualising treatment in adolescents requires consideration of several factors: clinical aspects of the disease including disease burden, frequency and severity of attacks, comorbidities; the impact on quality of life including missed school, interference with family life, daily functioning, and anxiety about future attacks; and broader practical concerns.2,19 Kinaciyan highlighted, “The most complicated thing is the other factors,” such as variable drug availability across regions.
Key Takeaways
The burden of HAE is substantial and extends beyond the frequency of attacks, significantly affecting QoL and treatment experiences. Personalised management through comprehensive consultations and shared decision-making is crucial to align care with individual patient goals. Regular review and, when appropriate, switching of LTP treatments can help optimise outcomes, especially for those who remain symptomatic or burdened by their current therapy. Additionally, recognising and addressing the unique needs and preferences of adolescents is vital to support their long-term wellbeing and enable a future free from the limitations of HAE.
UK. HAE.00251 July 2025




