BACKGROUND
Patients with hypertrophic cardiomyopathy (HCM) frequently reduce physical activity due to concerns about sudden cardiac death, though evidence for these restrictions is limited.1,2 Most data on activity in HCM rely on patient-reported measures, with little objective quantification or phenotype-specific analysis.3
METHODS
In this multicentre Dutch study,4 accelerometry was used to measure 7-day physical activity in 203 patients with HCM and 37 genotype-positive, phenotype-negative (G+/P–) relatives. G+/P– relatives were considered healthy controls. The primary outcomes were daily steps, time spent in moderate-to-vigorous physical activity, and sedentariness. Quality of life (QoL) was assessed using the Kansas City Cardiomyopathy Questionnaire (KCCQ) and the EuroQoL 5-dimension 5-level (EuroQoL-5D-5L) questionnaire. Subgroup analyses included symptomatic versus asymptomatic, obstructive versus non-obstructive, BMI groups, and medication use.
RESULTS
Physical activity in patients with HCM was significantly decreased. Patients with HCM walked fewer steps per day (5,254 versus 6,573). Furthermore, as displayed in Figure 1, these patients engaged in less moderate-to-vigorous physical activity (3.4% versus 4.5% of the day), and were more sedentary (>80% of waking hours: 61% versus 35%) compared with G+/P– individuals (all p<0.01). Patients who were symptomatic and those with left ventricular outflow tract obstruction had the lowest activity. While patients who were asymptomatic and non-obstructive were as physically active as healthy controls, strikingly, even patients who were asymptomatic and obstructive showed markedly reduced activity, comparable to individuals who were symptomatic. Obesity and the use of cardiac medications, particularly β-blockers, were associated with significant reductions in physical activity.5,6
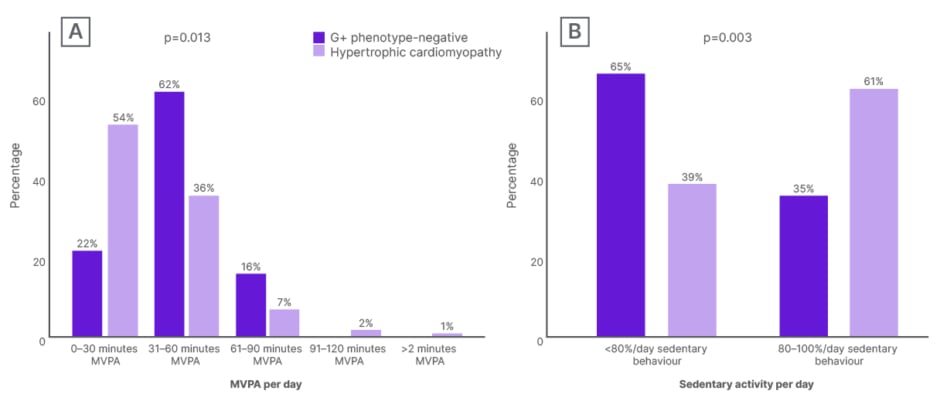
Figure 1: Physical activity and sedentariness.
A) Distribution of MVPA (min/day) in 30-minute increments. B) Distribution of sedentary behaviour (%/day) for participants who are G+ phenotype-negative and participants who have hypertrophic cardiomyopathy.
G+: genotype-positive; MVPA: moderate-to-vigorous physical activity.
Daily steps correlated with QoL, with every 250 step/day increase being associated with a 2.15-point higher KCCQ score, and every 1,000 step/day increase with a 0.05-point higher EQ-5D-5L score (both p<0.001). All associations remained significant after adjustment for age and sex. Lastly, more than half of patients recalled receiving previous exercise guidance from their cardiologist, and most reduced their activity as a consequence. However, objective activity measured with accelerometry did not differ between those who restricted their activity versus those who did not.
CONCLUSION
This is the largest multicentre accelerometry-based analysis in HCM that included G+/P– controls. Patients with HCM are substantially less active and more sedentary, especially if symptomatic, obstructive, or obese. Even modest increases in step counts were linked to clinically meaningful QoL improvements.7 These findings underline the need for individualised, phenotype-informed exercise counselling and careful reconsideration of restrictive advice, and support the integration of wearable data into clinical care and clinical trials.8-11







