BACKGROUND
Glucagon-like peptide-1 receptor agonists (GLP-1RA) are widely prescribed for Type 2 diabetes and obesity owing to their robust metabolic and cardiovascular benefits. Emerging reports, however, suggest a potential link between GLP-1RA use and non-scarring hair loss (NSHL), including telogen effluvium (TE), androgenic alopecia (AGA), and alopecia areata (AA). To clarify this association, the authors conducted the first large-scale, real-world multicentre cohort study evaluating GLP-1RA exposure and risk of hair loss (HL).1
METHODS
This retrospective analysis leveraged the TriNetX US Collaborative Network (2014–2024), comprising 67 healthcare organisations and >100 million patients. Adults (18–89 years) with ≥2 instances of GLP-1RA prescriptions (liraglutide, semaglutide, dulaglutide, exenatide, lixisenatide, or tirzepatide) were included. Patients with prior alopecia or confounding conditions, such as thyroid disease, ovarian dysfunction, menopause, malnutrition, chemotherapy, connective tissue disease, scarring alopecias, bariatric surgery, or trichotillomania, were excluded. Propensity score matching was performed for age, sex, race/ethnicity, BMI, and Type 2 diabetes status. HL outcomes were defined using the 10th version of the International Classification of Diseases (ICD-10) codes, with adjusted odds ratios (aOR) estimated at 6 and 12 months.
RESULTS
Matched adult cohorts (n=547,993 each) were well balanced (mean age: approximately 53 years; approximately 50% female; 65% White, 17–18% Black, 10% Hispanic/Latino; Table 1). From 2014–2024, the incidence of TE, AGA, and overall NSHL rose more steeply in GLP-1RA users compared with controls. At 6 months, GLP-1RA exposure was associated with increased risk of AGA (aOR: 1.62; 95% CI: 1.24–2.12) and overall NSHL (aOR: 1.26; 95% CI: 1.15–1.38), while TE and AA were non-significant. By 12 months, risk was significantly elevated for TE (aOR: 1.76; 95% CI: 1.34–2.32), AGA (aOR: 1.64; 95% CI: 1.35–1.99), and overall NSHL (aOR: 1.40; 95% CI: 1.31–1.49), with AA remaining non-significant.
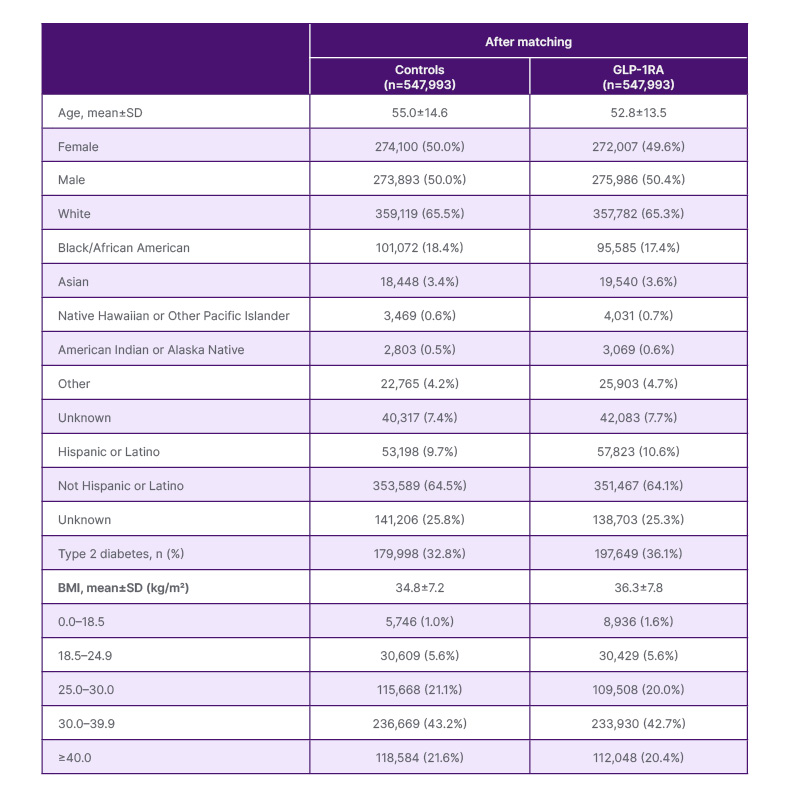
Table 1: Baseline demographic and clinical characteristics of glucagon-like peptide-1 receptor agonist users and controls before and after propensity score matching.
GLP-1RA: glucagon-like peptide-1 receptor agonist.
These findings align with pharmacovigilance signals from the FDA Adverse Event Reporting System (FAERS) and VigiBase, which reported increased odds of alopecia with semaglutide and tirzepatide.2,3 Proposed mechanisms include rapid weight loss precipitating TE, metabolic and hormonal shifts accelerating AGA, and possible direct follicular effects given GLP-1 receptor expression in hair follicles.4-6 In contrast, case reports have described improvement in scarring alopecias such as folliculitis decalvans and central centrifugal cicatricial alopecia with GLP-1RAs,7,8 suggesting divergent and complex biological pathways. Temporal trends further reinforce this signal: both cohorts experienced a spike in TE incidence around 2020, likely reflecting the impact of COVID-19, followed by a sustained rise among GLP-1RA users coinciding with the widespread adoption of semaglutide and tirzepatide.9
Together, these data support the authors’ recommendation that all patients initiating GLP-1RAs should be counselled regarding the potential HL risk. For those presenting with new-onset shedding, nutritional and endocrine evaluation should be prioritised, and early referral to dermatology may improve outcomes and adherence. Educating patients on HL risks prior to therapy initiation may help set expectations, promote timely reporting, and inspire exploration of potential methods to prevent TE in this setting.
CONCLUSION
In conclusion, GLP-1RA therapy was independently associated with increased incidence of TE, AGA, and overall NSHL in adults, but not AA. While causality cannot be established from observational data, this large, real-world dataset study provides compelling evidence of a clinically relevant signal, highlighting the need for monitoring, patient education, and further mechanistic investigation.







