Abstract
Psoriasis, a chronic inflammatory skin disease, presents treatment challenges, especially when complicated by conditions like venous insufficiency. While the Koebner phenomenon suggests trauma can worsen psoriasis, this case report describes a 41-year-old male patient with psoriasis vulgaris and venous insufficiency, who experienced complete remission of his psoriasis following endovenous laser ablation for his varicose veins. This unexpected outcome, beginning within weeks of the procedure and culminating in complete remission within 6 months, highlights the complex relationship between trauma and psoriasis. Potential explanations include a localised immune response, improved circulation, or a direct laser effect. This case underscores the need for further research into the interplay between venous insufficiency treatments and psoriasis activity, as understanding these mechanisms could inform future treatment strategies.
Key Points
1. This case highlights the potential for endovenous laser ablation (EVLA) to induce unexpected remission of psoriasis in patients with concurrent venous insufficiency. Clinicians should be aware that EVLA, while addressing vascular concerns, may offer unanticipated dermatological benefits, challenging the traditional view of trauma-induced psoriasis flares.2. While the Koebner phenomenon suggests trauma can exacerbate psoriasis, this case demonstrates a paradoxical outcome. EVLA, a controlled form of trauma, resulted in complete psoriasis remission, suggesting complex immunomodulatory effects. This case prompts clinicians to consider the nuanced relationship between trauma and psoriasis activity in vascular interventions
3. This report underscores the need for further research into the interaction between venous insufficiency treatments and psoriasis. Clinicians should be cognisant of the potential for EVLA to positively influence psoriasis. Further studies are warranted to explore the mechanisms behind this observation, potentially leading to novel therapeutic strategies for both conditions.
INTRODUCTION
Psoriasis, a prevalent chronic inflammatory skin disease affecting 2–3% of the global population,1 poses a significant therapeutic challenge. Characterised by well-demarcated erythematous plaques with adherent silvery scales, psoriasis vulgaris, the most common variant (85–90% of cases),2,3 significantly impacts patients’ quality of life.4 While topical corticosteroids remain a common treatment, long-term safety concerns limit their sustained efficacy.5 The complex, multifactorial pathogenesis of psoriasis involves genetic predisposition, environmental triggers, and immune dysregulation.6 Recent advances have led to targeted therapies for moderate-to-severe disease,7 but challenges persist, particularly in the lower extremities, where treatment is complicated by factors such as friction, dependent oedema, and potentially altered drug absorption.8 Furthermore, psoriasis can coexist with venous insufficiency, a common disorder. Venous insufficiency treatments, including thermal ablation, may induce the Koebner phenomenon (isomorphic response), exacerbating psoriasis.9 However, the relationship between trauma and psoriasis is not always linear. While trauma can trigger flares, controlled trauma may have therapeutic potential in certain contexts. For instance, Krefting et al.10 demonstrated that compression therapy in patients with psoriasis and lower extremity oedema did not worsen the skin condition and even suggested potential benefit, highlighting the complex interplay between pressure and psoriasis. In this case report, the authors present the unexpected remission of psoriasis following endovenous laser ablation (EVLA) for venous insufficiency in a patient with both conditions, and discuss the potential mechanisms underlying this observation.
CASE REPORT
A 41-year-old male patient presented with prominent, localised psoriasis vulgaris on his left lower extremity and scalp, accompanied by symptoms of venous insufficiency. Clinically, his psoriasis was characterised by well-defined, erythematous plaques with silvery scales. Concurrently, he exhibited classic signs of venous insufficiency, including oedema, pain, and visible varicose veins. Psoriasis vulgaris had been previously diagnosed based on its characteristic clinical presentation. Venous insufficiency was confirmed by both clinical signs and symptoms, with duplex ultrasound imaging further corroborating reflux in the great saphenous vein. No significant diagnostic challenges were encountered.
The patient had a 25-year history of psoriasis, during which he had undergone various topical and systemic therapies without achieving complete resolution. Notably, he was not receiving any specific treatment for his psoriasis immediately before or during the EVLA procedure. Given his dual diagnosis, treatment options for his varicose veins were carefully considered, particularly regarding the potential risk of the Koebner phenomenon. Non-thermal treatments, such as sclerotherapy and glue ablation, which carry a lower trauma potential, were thoroughly discussed. Ultimately, after a comprehensive review of the risks and benefits, the patient opted for EVLA, a thermal treatment, for his venous insufficiency. The procedure was performed using a Biolitec® ELVeS Radial 2ring fiber (Integrated Connection [IC], 1,470 nm; Biolitec AG, Jena, Germany).
Surprisingly, following the EVLA procedure, the psoriatic lesions on his left lower extremity achieved complete remission (Figure 1). This unexpected improvement began within a few weeks post-procedure and progressively advanced to full remission by the 6-month follow-up mark. During this period, the patient received a 3-month course of calcium dobesilate 500 mg twice daily for his venous insufficiency, after which the medication was discontinued. No changes were observed in the psoriatic plaques on the patient’s scalp throughout the follow-up period, indicating that the effect was localised to the treated area rather than systemic. The patient reported excellent tolerability to the EVLA procedure and adhered well to post-procedural care instructions. No adverse or unanticipated events directly related to the EVLA procedure were observed, apart from the remarkable and unexpected psoriasis remission itself.
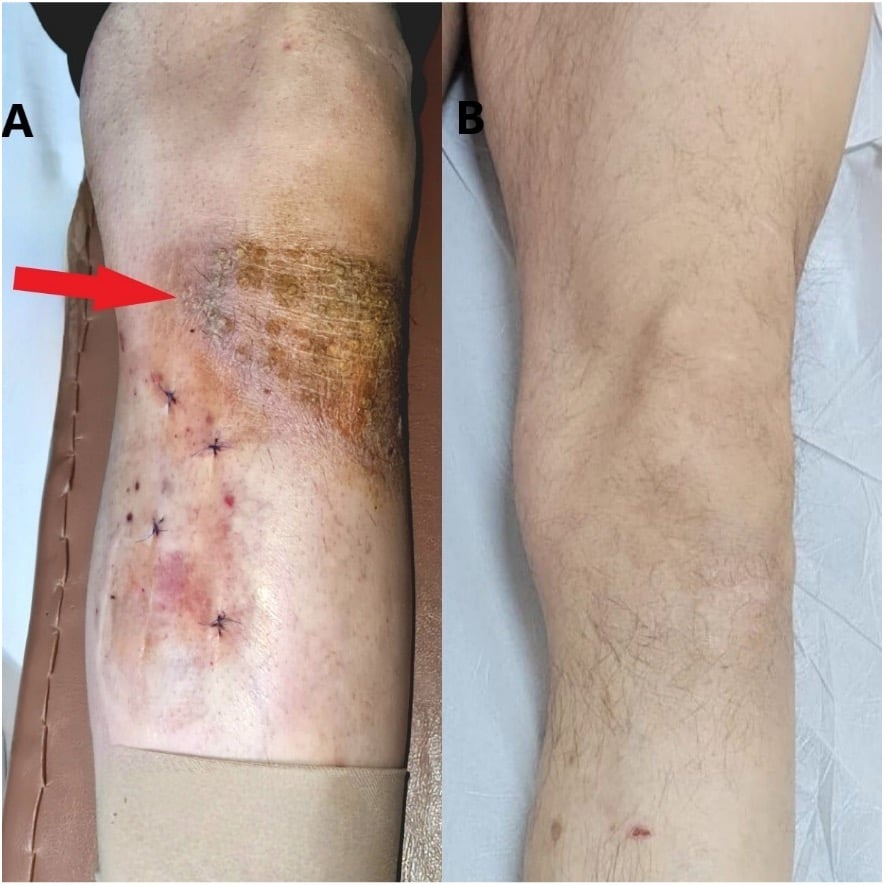
Figure 1: Post-operative images following endovenous laser ablation procedure.
A) Post-operative Day 1. This image shows the localised psoriasis (indicated by the red arrow) on the patient’s left lower extremity.
B) Six months post-operative. This image demonstrates complete resolution of the patient’s localised psoriasis on the left lower extremity.
DISCUSSION
To contextualise this case, a comprehensive literature search of PubMed, Embase, and Scopus using the keywords “Koebner phenomenon,” “lower extremity,” “psoriasis,” “EVLA,” and “management” revealed a notable absence of prior reports directly linking psoriasis remission to EVLA for venous insufficiency or similar atypical Koebner responses. This lack of literature underscores the novelty and potential significance of this observation as a rare, possibly first-documented instance. While the exact mechanisms remain unclear, EVLA may have exerted local immunomodulatory effects via reduced venous stasis. Interestingly, while the authors’ case demonstrates a surprising remission of psoriasis following EVLA, a recent systematic review and meta-analysis suggests that psoriasis is associated with an increased risk for incident venous thromboembolism and peripheral vascular disease.11 This highlights the complex and potentially bidirectional relationship between psoriasis and the vascular system, further emphasising the need for comprehensive research in this area.
This case shows the complex and sometimes counterintuitive relationship between trauma and psoriasis activity. While the Koebner phenomenon9 describes the risk of psoriasis flares following trauma, this patient experienced complete remission of his psoriasis after EVLA for venous insufficiency, a paradoxical outcome. Several potential mechanisms may explain this observation. EVLA, although a controlled form of trauma, may have triggered a localised immune response that inadvertently modulated the patient’s psoriasis. Alternatively, the improved venous circulation resulting from EVLA may have indirectly influenced the psoriasis, perhaps by reducing local inflammation or enhancing the delivery of topical or systemic medications. This concept aligns with findings from Krefting et al.,10 whose study on compression therapy suggests that controlled pressure or trauma may have a therapeutic role in some patients with psoriasis, supporting the notion that the relationship between trauma and psoriasis is not universally detrimental. Another possibility is a direct effect of the laser energy on the psoriasis. Given the use of laser therapy in treating psoriasis, the EVLA laser may have exerted a similar, albeit unintended, therapeutic effect.12,13 While non-thermal treatments for venous insufficiency, such as sclerotherapy, are available and also induce some degree of intentional vascular trauma, the literature regarding their impact on concurrent psoriasis is limited. The limited existing literature on this specific clinical scenario underscores the importance of future research to comprehensively evaluate the impact of venous insufficiency treatments on psoriasis activity. Well-designed studies are needed to determine the safety and efficacy of these interventions in patients with both conditions, and to clarify the biological pathways that may lead to atypical responses like the psoriasis remission seen in the authors’ case, ultimately guiding clinical decision-making.







