Interview Summary
Acne is a chronic inflammatory skin disease whose visible effects can have a significant psychological impact on patients. A multimodal approach to acne management is vital in order to target the four interlinked pathological processes that underpin this common skin condition. During interviews conducted by EMJ, Sandeep Cliff, Consultant Dermatologist at Surrey and Sussex University Healthcare Trust, and Alison Layton, Consultant Dermatologist from Harrogate and District NHS Foundation Trust, both in the UK, explored the burden, pathophysiology, and current and future landscape of acne treatment. Experts highlighted existing unmet needs in acne care and explained how therapeutic innovations, such as the novel androgen receptor inhibitor clascoterone, may help to reshape acne management in daily clinical practice moving forward.PATHOPHYSIOLOGY AND BURDEN OF ACNE
Acne is a chronic and inflammatory skin condition characterised by the presence of both comedonal and inflammatory lesions, primarily on the face but also affecting the chest and back.1 “It affects a significant number of patients at some time in their life,” noted Cliff. “Up to 70% of teenagers and young people have acne, but it can also affect older patients as well.”2
Layton explained that four pathophysiological pillars underpin acne development: excess sebum production, follicular hyperkeratinisation, colonisation and proliferation of Cutibacterium acnes (C. acnes), and inflammation.3 She elaborated: “Dysregulation of the sebaceous gland is very much androgen-mediated and driven by hormones, particularly at puberty.
Those androgens also produce abnormal epithelial proliferation and differentiation of keratinocytes within the intrafollicular duct, and that provides a really favourable milieu for anaerobic Cutibacterium bacteria, which proliferate and colonise. This results in both innate and adaptive immune responses, which lead to the typical inflammatory lesions we see in acne. Many of these are responses triggered by Cutibacterium acnes.”
Both experts emphasised the pivotal role of androgens in acne pathogenesis, with activation of androgen receptors leading to excessive sebum production in the skin (Figure 1).3 “Acne is centred around the pilosebaceous unit, which is responsible for driving the production of sebum onto the skin,” Cliff explained. “The principal problem with acne is that the pilosebaceous unit is producing lots of sebum and this, coupled with other changes, leads to the development of acne.”
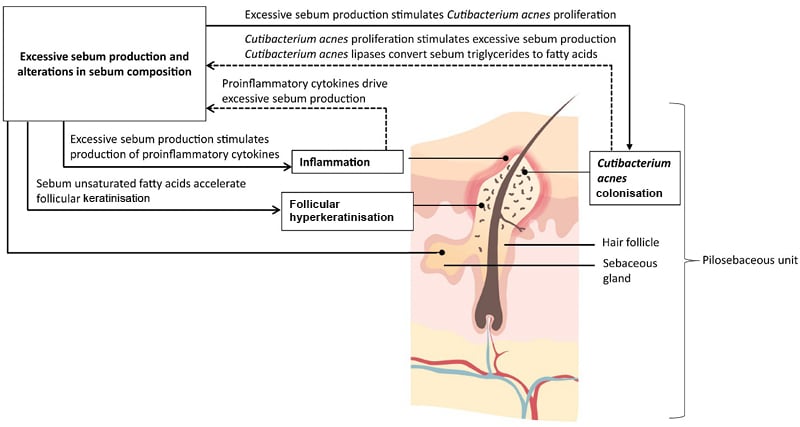
Figure 1: The contribution of sebum to acne pathophysiology.3
The primary role of sebum in the pathophysiology of acne vulgaris and its therapeutic relevance in acne management by James Q. Del Rosso & Leon Kircik ©2023 The Author(s), taken from Journal of Dermatological Treatment ©2023, © Taylor & Francis Ltd 2023, reprinted by permission of Informa UK Limited, trading Taylor & Francis Group, https://www.tandfonline.com.
Mental Health Impacts
Acne is associated with well-documented negative effects on quality of life and may prove emotionally devastating for adolescents at the stage of life when self-image is paramount.1 “Not only can acne itself have physical effects, it can be inflammatory, sore, painful, and weepy, but it has an impact on mental health as well,” stressed Cliff. “Low self-esteem can affect patients’ ability to function, and they can become depressed and have anxiety. So, it has a dual effect on patients, which I think is sometimes underestimated by many healthcare professionals and society at large.” The damaging psychological sequelae of acne were reiterated by Layton, who pointed to the results of a recent acne impact study that found that acne-related appearance concerns were associated with significant mental health issues, including depression, anxiety, and even suicide in some cases.4
Both experts blamed social media and today’s increasingly ‘cosmetic environment’ for heightening the negative impacts of acne. “For young people, their self-esteem comes from presenting themselves well on a day-to-day basis, which means anything that destroys their appearance can have a negative impact on their mental health,” explained Cliff.
Layton also noted that visible acne could be associated with significant stigmatisation and bias in how those affected are perceived by the wider population. “And, of course, the other big burden is that acne can go on to produce scarring,” Layton stated. “About 90% of patients will get some degree of scarring, and we have very few effective treatments for scarring, and in many cases it is permanent. In some patients, especially with skin of colour, we can see problems with hyperpigmentation, which again produces burden in its own right and is often long-lasting,” she explained.
TREATMENT LANDSCAPE AND UNMET NEEDS
The main treatment options for acne indicated for use in the UK are topical agents, oral antibiotics, and isotretinoin.5 Layton explained that fixed combination topical products are currently recommended as first-line options in the majority of leading acne guidelines, including the National Institute for Health and Care Excellence (NICE).5,6 “Some of the fixed combination products are actually licensed for moderate-to-severe disease and not just mild-to-moderate, so that’s our starting point, and then if patients are not responding, we would consider adding an oral antibiotic; however, there are concerns about using antibiotics for more than 6 months,” Layton outlined.
In the clinical practice setting, Cliff emphasised the importance of assessing the dominant feature of a patient’s acne and directing treatment according to the principal pathology. “For general management of acne, the idea is to reduce the skin’s oil production. However, if a patient has inflammatory lesions that are probably precipitated or provoked by bacteria, then you want to use anti-inflammatory agents, such as an antibiotic, which is given orally or topically,” he explained. “The advantage of that is it’s relatively easy for most patients to take a tablet or to apply a topical preparation. However for many young adults compliance can be a real issue, so effective treatments which have non complicated regimes are favourable in practice.”
For severe acne, experts agreed that isotretinoin is a highly effective therapeutic option. As Cliff described: “It is an oral retinoid that binds to the retinoid receptors in the pilosebaceous units and significantly reduces sebum production in the skin. It also reduces hyperkeratinisation, so it helps to stop the blockage of the pilosebaceous units, and by doing so, it is also thought to have an anti-inflammatory effect on the skin. So, it helps to reduce acne, sometimes definitively, sometimes temporarily.”
However, Cliff cautioned that isotretinoin is also associated with side effects such as teratogenicity and mood and behaviour changes, “some of which have only recently come to the surface”.7 “One should exert a degree of caution, I think, in patients who’ve got issues with mental health, and be careful when instituting isotretinoin. However, more data are coming through showing that isotretinoin itself does not induce depression and that not treating the acne effectively may do more harm than good, so it is important not to deter patients from what is a very effective treatment that is used widely in practice.” Cliff also noted that, despite clinicians continuing to advocate for the benefits of isotretinoin, patients themselves are now increasingly reluctant to try the drug given the negative media coverage of potential psychological adverse events. “The shoe is on the other foot now because patients, quite rightly, are making decisions about how they wish their care to be delivered,” he remarked. “So a good patient-clinician relationship is needed so that the most effective treatment is offered with the patient being fully informed in the decision-making process.”
Beyond these three key treatment modalities for acne, Cliff mentioned prescription preparations such as oral contraceptives and oral aldosterone antagonists, although he emphasised that these products are not currently licensed for acne in the UK. He also alluded to the range of other non-prescription topical acne products which are available over the counter.
The Importance of a Multimodal Approach
The need to adopt a multimodal approach to acne management in daily dermatology practice was emphasised by both experts. Cliff explained that acne has many different facets, including excess sebum production and inflammatory processes in the skin, which require different strategies to target effectively. “The approach must be multifaceted; otherwise, you will end up treating one component of the acne, not the whole package,” he insisted.
Layton suggested that the reason for isotretinoin’s unparalleled clinical efficacy may lie in its ability to either directly or indirectly impact all four of the main pathophysiological features of acne. “Isotretinoin has a multimodal mechanism of action in its own right,” she surmised. “But all these other treatments are just looking at one or two of the pathophysiological factors implicated in acne aetiology. So, in order to actually try and address all of them, we need to be using more than one therapy.”
Current Gaps in Acne Care
Considering the unmet needs that exist with current acne therapies, Cliff highlighted compliance, side effects, and lack of response/breakouts as essential issues. He explained that compliance is a particular challenge given the principally teenage patient population and that side effects of topical agents, such as bleaching with benzoyl peroxide (BPO) and skin drying with topical retinoids, can also further exacerbate this problem. “Patients do not want to use a product that, in their eyes, makes them look worse and feel worse than when they came to see us in the first place, so that’s where there is a definite vacuum that we need to address,” he remarked. Cliff also noted that patients require more effective treatment options to help manage occasional acne breakouts without resorting to ‘aggressive’ therapies such as antibiotics and isotretinoin.
On the subject of isotretinoin, Layton also highlighted the current ‘controversy’ around its positioning for acne treatment in the UK. “The Medicines and Healthcare products Regulatory Agency (MHRA) has reviewed the use of isotretinoin and has reminded prescribers that it is licensed for severe disease, including acne that is at risk of permanent scarring that has not responded to previous and adequate combination therapies,” she expounded.8 “So, there are numerous patients sitting in that moderate disease category that isotretinoin now isn’t licensed for.” The additional measures put in place by the MHRA include the need for two independent prescribers to agree on the initiation of isotretinoin in patients under 18 years, new counselling requirements about potential mental health and sexual function side effects, and assessment of mental health and sexual function before starting treatment, as well as monitoring during treatment.8
“There is also got a big problem with antibiotics,” Layton acknowledged. “As dermatologists, we’re one of the biggest offenders in terms of the number and duration of antibiotics we use. NICE guidance limits use to 6 months, but acne is a chronic disease, and the average duration is probably 6–7 years.5 So, if a patient’s acne deteriorates again when you stop antibiotics and is not controlled on topical therapies, it represents a real unmet need in terms of what we do with those patients.” Cliff also pointed to the increasing problem of antibiotic resistance, which is reducing patients’ responsiveness to antibiotic acne therapies and further underscores the need for novel treatment approaches.
Finally, both experts highlighted the need to address the excess sebum production, which is fundamental to acne pathogenesis. “One of the biggest unmet needs, I think, is that sebum is integral to acne, but until recently there was no topical agent specifically designed to reduce sebum,” Layton pointed out. “For males, we only have oral isotretinoin, which is licensed for severe acne and reduces sebum, but no topical agents. For females, we have things like oral aldosterone antagonists and oral contraceptive pills, but the majority are not licensed in the UK, so, there’s a real unmet need in terms of being able to reduce that sebum, which is so integral to the disease.”
TARGETING THE ANDROGEN RECEPTOR
Clascoterone cream 10 mg/g is a topical androgen receptor inhibitor recently granted a marketing authorisation in the UK for the topical treatment of acne vulgaris in patients aged 12 years and older.9 Although the exact mechanism of action of clascoterone for the topical treatment of acne vulgaris is not fully characterised, in vitro studies suggest that clascoterone binds with high affinity to the androgen receptor in sebocytes, inhibiting downstream androgen-stimulated gene transcription (in vitro findings may not necessarily reflect in vivo phenomena).10 Both experts described clascoterone’s mode of action as “unique”, being the first topical anti androgen agent that reduces sebum production and thus intervenes early in the acne cascade.
“It’s a really interesting agent because it’s an androgen inhibitor, so it’s acting at the receptor, which means that it prevents the active effects of androgens at the receptor site,” Layton explained. As Cliff elaborated: “Acne is strongly influenced by the male hormone testosterone in both men and women, the byproduct of which is dihydrotestosterone (DHT), which we think binds these androgen receptors and activates the sebum production, which in turn activates the inflammation and activates the keratinisation. The logical thing then is to block the androgen receptors.”
Layton added: “Clascoterone is a competitive inhibitor of the antigen receptor, and there have been some in vitro studies suggesting that it inhibits the downstream signalling of androgen-responsive genes.”10,11 “From a clinical perspective, it’s the only topical agent we’ve got that is specifically developed to reduce sebum,” he continued. Cliff concurred: “This is a different way of looking at acne, a different approach with a topical preparation.”
In terms of the type of patient who could benefit from clascoterone’s androgen-inhibitory effects, experts highlighted adolescents going through puberty and experiencing the associated testosterone surge that increases sebum levels in the skin. Layton also alluded to its potential utility in “adult female patients with hormonally driven perioral acne”. Cliff suggested that clascoterone could additionally be considered for those patients experiencing acne flare-ups, including both treatment-naïve patients with acne or those previously treated with isotretinoin “who want to target those [breakout] areas with a topical treatment locally to control the acne, rather than treat with oral agents that can upset their stomach”.
Ultimately, however, experts concluded that clascoterone could prove a useful addition to the acne treatment armoury for eligible patients aged 12 years and older. “Sebum is integral to acne, so it should be helpful in most suitable patients,” Layton emphasised.
Clinical Evidence for Clascoterone
Clascoterone was evaluated in two 12-week, randomised, vehicle-controlled Phase III trials and a 9-month safety extension study; in the 12-week studies, it demonstrated superior efficacy to vehicle creams.9,12-14 “From the clinical perspective, the big studies are the two pivotal multinational, multicentre studies,” Layton confirmed. “Over 12 weeks, clascoterone showed good efficacy in terms of getting clear, or almost clear, skin in the majority of patients.” These two Phase III trials of clascoterone enrolled a total of 1,440 patients (males and females aged 9 years and older) with moderate or severe facial acne (Table 1).13 At Week 12, the treatment success rate, defined as an Investigator’s Global Assessment (IGA) score of 0 (clear) or 1 (almost clear) and a ≥2-grade improvement from baseline and absolute change from baseline in non-inflammatory and inflammatory lesion counts, was 18.8% with clascoterone versus 8.7% with vehicle in trial 1 and 20.9% with clascoterone versus 6.6% with vehicle in trial 2 .9
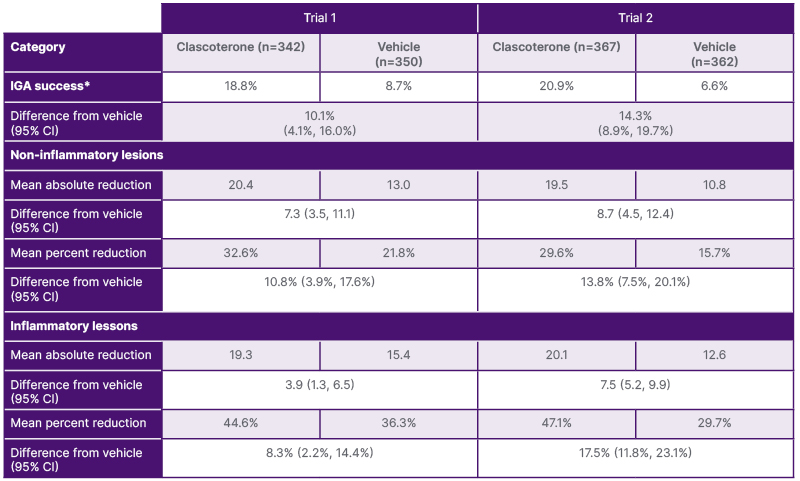
Table 1: Clinical efficacy of clascoterone in subjects with acne at Week 12.9
*IGA success was defined as at least a 2-point reduction in IGA compared to baseline and an IGA score of 0 (clear) or 1 (almost clear).
IGA: Investigator Global Assessment.
“The data from the short-term study, compared to vehicle, was significant in terms of the effectiveness and the reduction in inflammatory count or number of acne lesions, both by patient assessment and also by IGA,” remarked Cliff. “Enrolled patients had quite a large number of inflammatory lesions, and the results were significant,” he continued.
Experts also pointed to encouraging results from the open-label, long-term safety extension study that enrolled 609 patients who either continued existing treatment with clascoterone or switched to clascoterone from vehicle. In this study, in which clascoterone was applied twice daily for up to a further 9 months, a low frequency of treatment-emergent adverse events was observed.12 “We all worry if the treatment is safe enough to continue in the long term,” Cliff explained. “These data showed clascoterone is generally well tolerated, which is paramount for our patients.”
In terms of clascoterone’s overall safety and tolerability profile in clinical studies, this was viewed favourably by both experts. “Although some patients did get some irritation and a bit of redness, by and large, the side effect profile was low and therefore positive from that angle,” said Cliff. “In all of the studies where clascoterone has been used in Phase III and IV studies, the main side effects have been local skin reactions, dryness, scaling, and redness, very much like you get with a lot of topical agents,” Layton confirmed.
EVOLUTION OF ACNE MANAGEMENT
Clascoterone in Clinical Practice
Based on these Phase III trial findings, experts discussed the potential value of clascoterone within the existing acne treatment armamentarium. Cliff described the clinical data as “convincing” and sufficient to support “definite benefits” for clascoterone used as a topical cream for patients experiencing acne flare-ups.
“We have here, potentially, a licensed product that blocks the androgen receptor on the pilosebaceous unit, which is where the whole process of acne is going on,”
Cliff elaborated. “This is a different modality of treatment, it’s not a retinoid, not a topical antibiotic, it’s an androgen receptor blocker.”
Layton added that: “One of the major advantages of clascoterone is actually having something you can use in boys as well as girls, and there are reports that have suggested it can be used in all ethnicities and skin of colour.” She also noted the potential utility of clascoterone in people undergoing gender transitioning who may be taking testosterone supplements, which can drive acne development. “Something that might be helpful in terms of reducing the sebum production would be useful in these patients as well,” she elaborated. “So, that’s another clinical area where I think clascoterone could be useful.”
The Future of Acne Care
Looking to the future of acne management, Layton highlighted exciting new advances in microbiome research, modulating the skin’s microbiome to increase the microbial diversity that is lost during acne development, and the potential role of therapeutic and preventative vaccines. She also suggested some interesting avenues for future research, such as the potential impact of early topical treatment on acne evolution.
In terms of acne treatment itself, Cliff acknowledged this has “been pretty flat” for the past 10–12 years and lacks any significant innovation. “While we’ve seen new products like new retinoids come on the market, we haven’t seen any new avenues to address acne through a different modality,” he remarked. “Clascoterone is the first in that respect, so it’s a potential game changer from that perspective.”
Cliff went on to highlight specific areas where clascoterone may fit into the current landscape of acne treatments and help to advance future clinical care. He suggested it may be beneficial in treating unpredictable, localised flare-ups of acne that are pustular or comedonal in nature, adding, “particularly for a hormonal flare-up or possibly for patients with polycystic ovaries.”
Cliff also described clascoterone as a potentially useful alternative “for patients who don’t want to take antibiotics because of potential side effects, or who don’t want to take isotretinoin for whatever reason.” However, he cautioned that the availability of this topical anti-androgen would augment, rather than supplant, existing options in the acne toolkit, particularly for severe disease. “If a patient has aggressive, cystic acne that is scarring, no topical agent is going to be effective because they need systemics, they need isotretinoin, and there’s no substitute for that,” he stressed.
Layton reiterated that a move away from antibiotics should be a top priority for acne care going forward. “We definitely need to find new ways of treating people which don’t involve antibiotics because we’ve got patients on antibiotics for years, and we’re often using things like doxycycline, which are important for other diseases,” she stressed. “So, if we’ve got new topicals that can be used as part of a regimen or on their own, that’s really important.”
For female patients of all ages, Layton also emphasised the need for new treatment options. “With earlier menarche, we’re seeing acne earlier, and having well-tolerated topical therapies that we could use early on in the onset of acne, I think, is really important,” she stressed. “And then also at the other end of the spectrum for hormonal acne, where we’re seeing adult females with persistent disease.”
“Given the restrictions on isotretinoin, having a topical therapy that can be used as part of a multimodal system is really important,” Layton pointed out. “The fact that clascoterone reduces sebum, and that’s so important in acne, means that all suitable patients potentially could benefit from it. It can be used as monotherapy but also as part of a multimodal treatment regimen as well.”
Cliff concurred that the scope for the use of topical antiandrogen in daily clinical practice could be substantial. “Many patients with mild to moderate acne could benefit from this kind of modality,” he concluded.
| Adverse events should be reported. Reporting forms and information can be found at yellowcard.mhra.gov.uk. Adverse events should also be reported to [email protected] or call 0800 458 0383.. |
Job Code: PP-UK-WIN-0008
Date of Prep: June 2025







