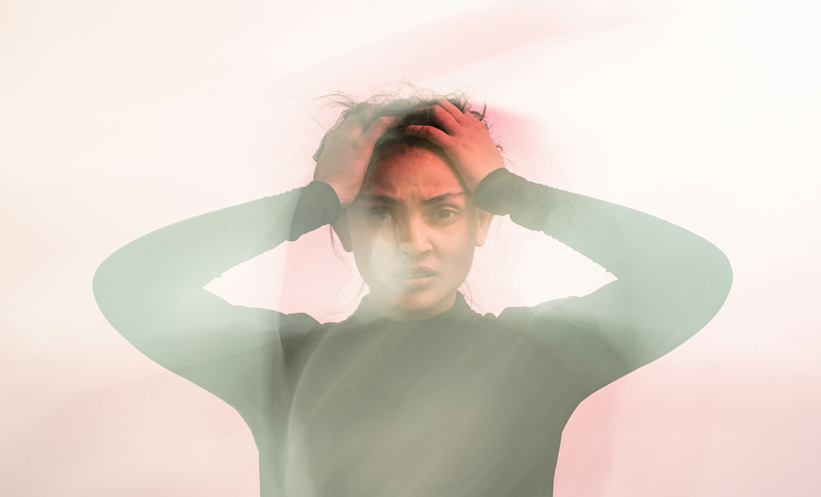
CHRONIC exposure to systemic inflammation may be associated with a greater risk of affective disorders, according to evidence from 1.5 million participants in the newly launched UK-wide Our Future Health research cohort. While it was already known that chronic inflammation could lead to an increased risk of psychiatric disorders, these data suggest that the risk of depression, bipolar disorder, and anxiety is nearly twice as high in people with autoimmune conditions, compared to the general population.
As there are no direct measurements of inflammation, the team considered the presence of an autoimmune condition, including Graves’ syndrome, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, lupus, and psoriasis, to be an indirect indicator of exposure to chronic inflammation. A total of 1,563,155 participants in the cohort provided sociodemographic, personal, and health and lifestyle information through a baseline health questionnaire. This included self-reported diagnoses for a range of disorders, including both psychiatric and autoimmune disorders, as well as the nine-item Patient Health Questionnaire and seven-item Generalised Anxiety Disorder Scale.
Results showed a significantly higher prevalence of any affective disorder in those with autoimmune conditions (28.8%) than the general population (17.9%). Looking at individual affective disorders, lifetime prevalence of depression was 25.5% in those with autoimmune disorders, versus 21.2% in the general population; prevalence of anxiety was 21.2% versus 15.2%, respectively; and prevalence of bipolar disorder was 0.9% versus 0.5%, respectively. Furthermore, significantly more current depressive and anxiety symptoms were present among those with autoimmune conditions. Researchers also noted that the risk of affective disorders was greater in females than in males with the same health conditions (31.6% versus 20.7%), except in people with lupus or rheumatoid arthritis, where there was no difference.
The study demonstrates the importance of regular screening for mental health conditions in those affected by autoimmune disorders, to enable early detection and provide tailored interventions. Since this observational study could not confirm potential causal mechanisms, such as fatigue, chronic pain, or social isolation, future research is needed to investigate these.
Reference
Mudra Rakshasa-Loots et al. Affective disorders and chronic inflammatory conditions: analysis of 1.5 million participants in Our Future Health. BMJ Ment Health. 2025;28:1-7.