BACKGROUND
Mitral valve transcatheter edge-to-edge repair (M-TEER) has transformed the treatment of mitral regurgitation (MR) for high-risk patients. However, 30–50% of patients fail to achieve ventricular and/or symptomatic recovery, and treatment response heterogeneity is poorly understood. STRESS-MR1 examines the acute and medium-term effects of M-TEER, through invasive characterisation of biventricular physiology and subsequent impact on recovery.
METHODS
STRESS-MR (St Thomas’ Hospital, London, UK; Royal Brompton Hospital, London, UK; and Oxford Heart Centre, Oxford, UK) is a UK multi-centre prospective study enrolling 53 consecutive patients between 2022–24 with primary MR (PMR; n=31) and secondary MR (SMR; n=22) undergoing M-TEER. Invasive biventricular pressure-volume loop (PVL) analysis and right heart catheterisation were performed immediately pre- and post-M-TEER. Serum biomarkers (troponin I, NT-proBNP) and 3D echocardiography were assessed at baseline, post-procedure, and 6-month follow-up. New York Heart Association class and Kansas City Cardiomyopathy Questionnaire scores were measured at baseline and at 6 months.
RESULTS
Whole cohort analysis demonstrated that deterioration of load-independent indices of right ventricular (RV) systolic function (end-systolic elastance [Ees]) and dyssynchrony following M-TEER were associated with the composite endpoint of cardiovascular death (CVD) and heart failure hospitalisation (HFH). A fall in left ventricular (LV) haemodynamic efficiency (the stroke work to pressure-volume area ratio [SW/PVA]) was associated with increased symptom burden (NYHA class ≥3) at follow-up. At baseline, patients with SMR demonstrated significantly lower LV ejection fraction (52% versus 68%; p<0.001), lower invasive ventriculo-arterial coupling (Ees/Ea) (1.07 versus 1.81; p<0.002), and lower SW/PVA (0.58 versus 0.74; p<0.001) compared to patient with PMR. Patients with PMR also saw greater improvements in intraprocedural cardiac index (CI) (0.5 versus 0.3 L/min/m2; p=0.011; Figure 1).
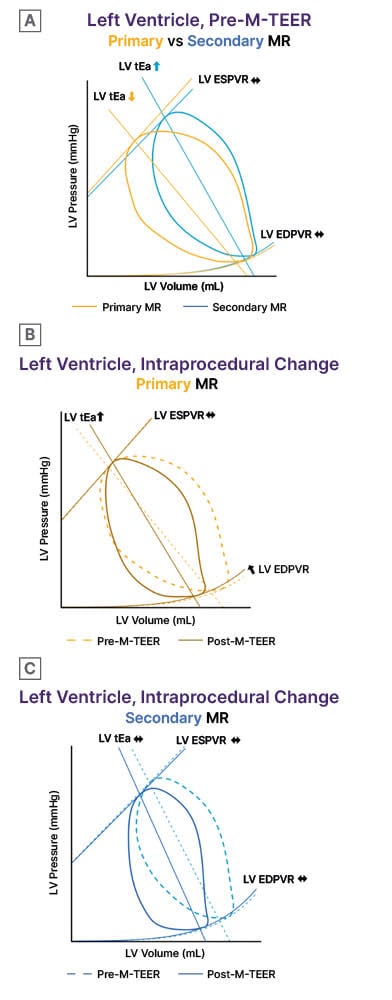
Figure 1: Representative left ventricular pressure-volume loops of primary and secondary mitral regurgitation patients pre- and post-mitral valve transcatheter edge-to-edge repair.
A) At baseline, patients with secondary MR had significantly higher total afterload and worse ventriculo-arterial coupling. Patients with secondary MR also had worse systolic function on certain indices (ejection fraction and preload recruitable stroke work).
B) Interprocedurally, patients with primary MR had significant decreases in ventricular compliance, as evidenced by the leftward shift in EDPVR. Patients with primary MR also saw greater increases in total afterload but also had improvements in ventriculo-arterial coupling.
C) Patient with secondary MR did not see significant changes in diastolic function. Patients with secondary MR also saw no significant changes in afterload or ventriculo-arterial coupling.
EDPVR: end-diastolic pressure-volume relationship; ESPVR: end-systolic pressure-volume relationship; LV: left ventricle; MR: mitral regurgitation; M-TEER: transcatheter mitral edge-to-edge repair; RV: right ventricle; tEa: total afterload.
When investigating the relationship between MR reduction and cardiac physiology, an intraprocedural reduction in 3D vena contracta area of >80% yielded a significant fall in CI (p=0.043) and RV Ees (p=0.025). Furthermore, a 4-grade reduction in MR to Grade 0 yielded no improvement in LV SW/PVA (p=0.22) and a fall in Ees/Ea (β: –0.38; p=0.02).
Haemodynamic responders (defined as an intraprocedural increase in CI) saw improvements in LV Ees/Ea (0.15 versus –0.07; p=0.006) and a reduced incidence of CVD/HFH compared to non-responders (7.4% versus 38%; p=0.007). Patients with a ≥10% reduction in LV end-diastolic diameter had greater improvements in CI (0.68 versus 0.23; p=0.008) and pulmonary artery systolic pressure (–10 versus –1; p=0.006) compared to non-remodelers. Finally, a ≥10-point increase in Kansas City Cardiomyopathy Questionnaire score was associated with greater improvements in CI (0.46 versus 0.22 L/min/m2; p=0.048), RVSW/PWA (0.54 versus 0.36; p=0.013), and Ees/Ea (0.69 versus 0.34; p=0.006).
CONCLUSION
Deterioration in LV efficiency, RV systolic impairment, and dyssynchrony following M-TEER increases the risk of CVD/HFH, and symptom burden. Patients with PMR and SMR have very distinct baseline physiologies and those with SMR demonstrate less improvement in CI, remodelling, and functional recovery. The authors have also identified an MR reduction threshold beyond which some patients exhibit deterioration in CI and biventricular haemodynamic performance.
This heterogeneous response to M-TEER highlights the importance of the heart team considering physiological suitability alongside anatomical assessment in identifying the right treatment approach for the right patient.







