BACKGROUND
Percutaneous coronary intervention (PCI), guided by physiological lesion assessment, has been shown to improve clinical outcomes by optimising the selection and treatment of ischaemia-related stenoses.1,2 Drug-eluting stents (DES) remain the cornerstone of PCI, yet drug-coated balloons (DCB) offer an attractive alternative in specific clinical contexts, particularly where stent avoidance is desirable, such as diffuse disease, bifurcation lesions, and high bleeding risk patients.3 Despite growing evidence for DCB efficacy, their role in physiology-guided PCI strategies remains underexplored. This study aimed to compare the safety, efficacy, and clinical outcomes of physiology-guided DCB-PCI versus DES-PCI using real-world, propensity-matched data.4
METHODS
This analysis was derived from the post-revascularisation optimisation and physiological evaluation of intermediate lesions using fractional flow reserve (PROPHET-FFR) registry,5 an ambispective registry that included patients with coronary lesions evaluated through functional testing. Starting from patients undergoing physiology-guided PCI with both pre- and post-PCI functional assessment, patients were divided into two groups according to the device used to perform physiology-guided PCI: DES versus DCB. Retrospective data provided the functionally DES-PCI cohort (FS-PCI), while prospective data included patients undergoing physiology-guided DCB-PCI (FB-PCI). All patients had pre- and post-PCI functional assessment with fractional flow reserve (FFR). In the DCB group, physiological guidance extended beyond lesion selection, incorporating functional reassessment after lesion preparation and prior to balloon delivery to confirm the appropriateness of a DCB-only approach. Propensity score matching (1:1) was performed using four variables: pre-PCI FFR values, clinical presentation (acute versus chronic coronary syndrome), lesion location in the left anterior descending artery, and follow-up duration. The primary endpoint was the rate of major cardiovascular events (MACE), defined as a composite of all-cause mortality, myocardial infarction, and target vessel revascularisation.
RESULTS
A total of 180 patients undergoing FS-PCI and 40 patients undergoing FB-PCI were initially screened. Following matching, 39 patients were included in each group. Baseline characteristics were well balanced in terms of age (p=0.357), male sex (p=0.329), diabetes (p=0.109), and clinical presentation (p=0.99). Conversely, hypertension (p=0.018), prior myocardial infarction (p=0.012), and previous PCI (p<0.01) were more prevalent in the DCB group. The DCB group also exhibited a lower left ventricular ejection fraction (54.1±8.6% versus 58.5±7.1%; p=0.016). Lesion location did not differ significantly (left anterior descending artery: 71.8% versus 83.0%; p=0.282). However, lesion morphology reflected clinical practice: in-stent restenosis was more frequent in the DCB group (53.8% versus 5.1%; p<0.001), while de novo lesions predominated in the DES group (94.9% versus 46.2%; p<0.001). The mean diameter of DCB and DES devices were similar, and close to 3 mm (2.98±0.41 mm versus 3.13±0.35 mm, respecively; p=0.132), indicating treatment of medium-caliber vessels. In contrast, device length was significantly shorter in the DCB group (26.7±7.6 mm versus 38.3±16.7 mm; p<0.01), suggesting a more conservative therapeutic approach. Pre-PCI FFR values were comparable (0.72±0.11 versus 0.74±0.07; p=0.398). Pressure microcatheters were more frequently used in the DCB group (76.9% versus 35.9%; p<0.01), likely reflecting caution to avoid rewiring following lesion preparation in the presence of possible dissections. Conversely, pressure wires were more commonly used in the DES group (23.1% versus 64.1%; p<0.01).
Although post-PCI FFR was lower in the DCB group (0.89±0.05 versus 0.91±0.04; p<0.01), at a median follow-up of approximately one year, there was no significant difference in the occurrence of the primary composite endpoint (2.6% in the DCB group versus 7.6% in the DES group; p=0.304), which was driven exclusively by target vessel revascularisation. No cases of all-cause mortality or myocardial infarction were observed in either group (Figure 1A). The incidence of periprocedural myocardial infarction was also comparable (2.6% versus 0%; p=0.314) (Figure 1B). Notably, only one case of bail-out stenting occurred following physiology-guided DCB-PCI, underscoring the procedural safety of this approach.
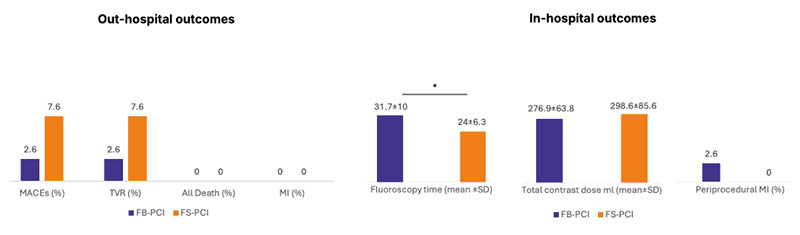
Figure 1: Out-of-hospital and in-hospital outcomes following functionally guided drug-coated balloon versus drug-eluting stent percutaneous coronary intervention.
* indicates p<0.05
FB-PCI: functionally guided drug-coated balloon percutaneous coronary intervention; FS-PCI: functionally guided drug-eluting stent percutaneous coronary intervention; MACE: major cardiovascular events; MI: myocardial infarction; TVR: target vessel revascularisation.
CONCLUSION
In this propensity-matched analysis, physiology-guided DCB-PCI was associated with clinical outcomes that were comparable to those of physiology-guided DES-PCI. These findings support the potential role of functionally guided DCB-PCI as a viable and safe alternative to stent implantation in appropriately selected patients, warranting further prospective investigation.







