BACKGROUND
Complex, high-risk percutaneous coronary interventions (PCI) are increasingly being performed in patients with non-ST-elevation acute coronary syndromes (NSTE-ACS). The British Cardiovascular Intervention Society (BCIS) has developed the complex high-risk and indicated PCI (CHIP-PCI) score, which is a valuable risk stratification tool for non-emergency PCI. A total of 13 factors, each scoring different points based on the observed odds-ratios, were independently associated with in-hospital major adverse cardiac and cerebrovascular events (MACCE), used as a marker of complexity after PCI. Seven patient factors (age ≥80 years, female sex, prior stroke, prior myocardial infarction (MI), peripheral arterial disease, left ventricle ejection fraction ≤30 %, chronic kidney disease) and six procedural factors (left main PCI, 3-vessel PCI, dual arterial access, left ventricle mechanical support, lesion length >60 mm, rotational atherectomy) were ultimately included in the CHIP-PCI score.1 According to another cohort study of more than 20,000 patients, CHIP-PCI score also showed promising results in predicting MACCE at one year. The authors sought to evaluate this score in patients with NSTE-ACS in clinical practice.2
METHODS
The authors retrospectively enrolled 356 consecutive patients with NSTE-ACS who underwent PCI from a single-centre cohort.3 Patients presenting with cardiogenic shock were excluded. The primary outcome was in-hospital MACCE, defined as a composite of all-cause death, periprocedural MI, or stroke. Additionally, bleeding complications and acute kidney injury (AKI) were included in the secondary endpoints. The patients were divided into four groups according to the BCIS CHIP-PCI score: group 1 (score 0), group 2 (score 1–2), group 3 (score 3–4) and group 4 (score ≥5, high-risk patients).
RESULTS
The mean age of this study population was 67±12 years, whereas the mean BCIS CHIP-PCI score was 1.92±2.1. Prior MI (37.4%), female sex (18.3%), and total stent length ≥60 mm (16.6%) were the most frequently met CHIP factors in this study. After calculating the BCI-CHIP score, 95 (26.7%), 149 (41.9%), 70 (19.7%), and 42 (11.8 %) patients were finally categorised into groups 1, 2, 3, and 4, respectively. In-hospital MACCE occurred in one patient (one MI, 1%) in group 1; three patients (two deaths, one MI, 2%) in group 2; and two patients (one MI, one stroke, 2.8%) in group 3. In patients with BCIS CHIP-PCI score ≥5, four primary events (three deaths and one stroke, 9.5%) were recorded (p<0.05).
Concerning secondary endpoints, two cases of major bleeding (retroperitoneal haematoma in group 1 and upper gastrointestinal bleeding in group 4), both treated with blood transfusions, were reported. One patient with a BCIS CHIP-PCI score of 1 had minor bleeding (severe bruising after aspirin and ticagrelor combination; switching from ticagrelor to clopidogrel led to clinical improvement). However, the difference in the occurrence of bleeding complications was not statistically significant (p=0.247). Also, a total of 20 cases of AKI (four in group 1, three in group 2, eight in group 3 and five in group 4) were reported. The number of patients with AKI was greater in groups 3 and 4 compared to groups 1 and 2(p<0.05; Table 1).
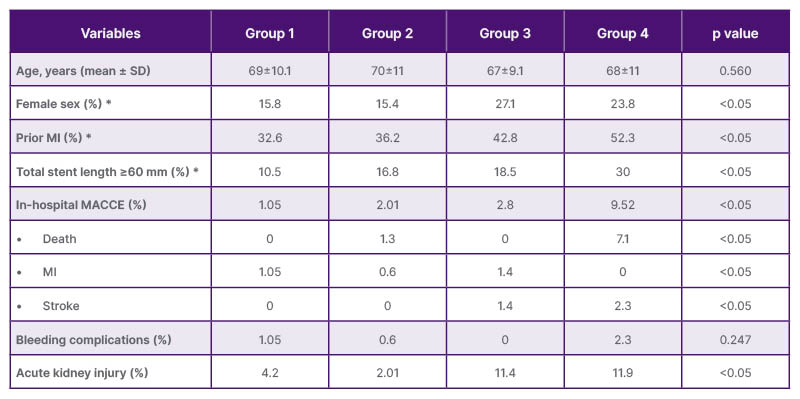
Table 1: Baseline characteristics and outcomes.
*most frequently met CHIP factors.
CHIP: complex and high-risk intervention in indicated patients; MACCE: major adverse cardiac and cerebrovascular events; MI: myocardial infarction.
CONCLUSION
Calculation of BCIS CHIP-PCI scores is feasible and offers a tailored approach in the management of patients with ACS who undergo a non-primary or emergency PCI. The risk of MACCE increases with higher score values. Moreover, early detection of risk factors for MACCE could improve in-hospital outcomes.







