BACKGROUND AND AIMS
Mycoplasma pneumoniae (MP) causes approximately two million infections in the USA,1 with increasing rates reported globally in the past few years.2-4 Rates in children have increased from 1.0 to 7.2% among those aged 2–4 years, and from 3.6 to 7.4% in those aged 5–17 years.1 In Illinois, USA, MP rates are about 5.1%, which is higher than rates of respiratory syncytial virus, influenza, or COVID-19.3 While MP usually presents as ‘walking pneumonia’ in school-aged children, there have been increases in extrapulmonary manifestations. The authors propose a severity scoring system for MP based off of the Westley Croup Score (WCS) and Phoenix Sepsis Criteria (PSC).5 Both have assessments of neurologic status. The WCS assesses degrees of respiratory distress, while the PSC assesses vitals and state of inflammation.
MATERIALS AND METHODS
To examine temporal trends in pediatric MP positivity rates, the authors aggregated counts, the total number of pediatric respiratory panel tests (PCR) ordered by year, and the count of positive MP results. Rates of MP positives per 1,000 tests were modeled using Poisson regression with the log of the number of respiratory panel tests included as an offset to adjust for variation in testing volume. Similar analyses describing time trends in MP hospitalization were not possible due to the infrequency of this event.
To identify factors associated with risk of being hospitalized for MP, the authors identified positive cases of MP in the electronic health record and conducted a chart review identifying demographics (sex, race, ethnicity, age), clinical findings (platelets, O2 requirements, respiratory distress defined as difficulty breathing, presence of retractions, tracheal tugging, head bobbing or grunting on physical exam, skin findings, and mental state), and year of infection. The authors used Chi-squared tests for categorical variables and t-tests for continuous variables. Factors significant on univariate analyses were included in multivariate analyses.
Statistical significance was defined as p<0.05. All analyses were conducted in R version 4.3.2.
RESULTS
The number of respiratory panels ordered, the number of MP cases, and the number of hospitalized MP cases all increased over the study period, though MP cases remained a small proportion of overall respiratory panels, peaking at 1.1% in 2024 (Table 1). At the start of the study period, the rate of positive MP cases was approximately 1.3 per 1,000 respiratory panel tests. Over time, the rate increased by about 6.5% per year (incidence rate ratio: 1.065; 95% CI: 1.014–1.120), after adjusting for testing volume.
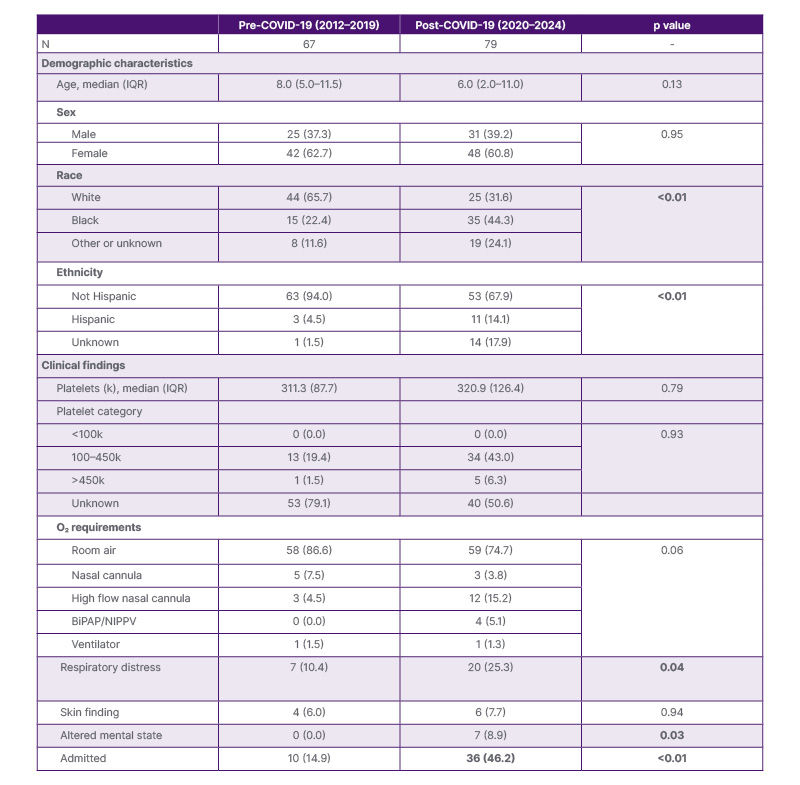
Table 1: Population characteristics pre- (2012–2019) and post- (2020–2024) COVID-19 pandemic.
Bolded p values indicate statistical significance (p<0.05).
BiPAP: bilevel positive airway pressure; IQR: interquartile range; NIPPV: non-invasive positive-pressure ventilation.
On univariate analysis, younger age, Black race, O2 requirements, respiratory support, altered mental state, and time-period (both pre- and post-COVID-19 pandemic and all other years versus 2024) were statistically significantly associated with greater odds of hospitalization. In multivariate analysis, Black race, respiratory distress, and time-period (both pre- and post-COVID-19 pandemic and all other years versus 2024) remained statistically significantly associated with greater odds of hospitalization.
CONCLUSION
Age, respiratory support, and altered mental status were all statistically significant predictors of MP severity. Younger, minority patients were more likely to be admitted. 2024 showed a statistically significant increase in both the number and severity of MP cases. More surveillance is needed in the USA to determine how prevalent and severe MP is in the pediatric population now and in the future.







