Abstract
Background: The emergency department (ED) plays a crucial role in addressing improper antibiotic prescribing, which is essential for reducing antimicrobial resistance (AMR) and preventing harm to patients. The increased use of oral azithromycin for treating community-acquired pneumonia (CAP) in the ED highlights the need for this study.
Objectives: To describe the prescribing practices and assess the appropriateness of oral azithromycin prescribing for CAP treatment in the ED of a tertiary hospital.
Methods: This retrospective observational study included patients aged 18 years and older who presented to the ED with CAP and were prescribed oral azithromycin.
Results: A total of 165 patients were enrolled, with 53.3% being female and under 65 years old. The majority (83.6%) had at least one comorbidity, with hypertension being the most prevalent (63.6%). Two-thirds of patients had a CURB-65 score of less than 2. A 3-day course of oral azithromycin (500 mg once daily) was the most frequently prescribed regimen (67.9%), while intravenous (IV) amoxicillin/clavulanate was the most administered concurrent antibiotic (69.3%). Among the 118 hospitalised patients, a CURB-65 score of less than 2 was the main reason (21.6%) for discontinuing oral azithromycin. Approximately 74% of prescriptions complied with national guidelines, with non-adherence primarily due to inappropriate treatment choices for outpatients without comorbidities. Guideline adherence was significantly higher in patients aged 65 or older and those with comorbidities.
Conclusion: Oral azithromycin prescribing adherence for CAP in the ED was moderate, with compliance rates in similar studies ranging from 7% to 95%, underscoring the need for strengthened antimicrobial stewardship programmes.
Key Points
1. Oral azithromycin prescribing surged in the Emergency Department (ED), raising concerns about inappropriate use. This study supports antimicrobial stewardship efforts to curb resistance, improve safety, and enhance treatment guideline compliance.2. This retrospective study assessed oral azithromycin prescribing practices for community-acquired pneumonia in a Malaysian tertiary hospital ED, examining compliance with national guidelines and associated patient outcomes.
3. While most oral azithromycin prescriptions were guideline-compliant, inappropriate use for low-risk patients persists. Strengthening antimicrobial stewardship in EDs is essential to improve prescribing practices and combat antimicrobial resistance.
INTRODUCTION
Azithromycin is an azalide effective against streptococci, staphylococci, Haemophilus spp., Moraxella spp., Neisseria gonorrhoeae, Legionella, Chlamydia spp., and Mycoplasma spp.1 Its broad spectrum, favourable safety profile, and ease of use make it an attractive option for treating community-acquired infections, especially acute respiratory infections. It is the initial empirical treatment of choice for community-acquired pneumonia (CAP) due to its action against atypical organisms such as Legionella, Chlamydia, and Mycoplasma.2,3 A meta-analysis showed that empirical atypical coverage was linked to lower clinical failure rates in hospitalised adults with CAP.4
Since the aetiological diagnosis is frequently not accessible at the outset, the selection of empirical antibiotic therapy for CAP is determined by the severity of the patient’s condition, which can be assessed using scoring systems like CURB-65.5 Prompt administration of the right antibiotics in the emergency department (ED) is crucial and can be life-saving, especially in cases of severe sepsis and septic shock.6 The Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) CAP treatment guidelines recommend that for patients admitted via the ED, the first dose of antibiotics should be administered prior to hospital admission.7 However, in cases of CAP and other infectious diseases, the unnecessary or improper use of antibiotics can result in harm to both patients and the community, including adverse events, treatment failures, and the development of antimicrobial resistance (AMR).8–10
Despite the widespread use of azithromycin, no audits to date have specifically targeted this drug in the ED. The trend in oral azithromycin prescribing, particularly the tablet dosage form, has shown an increase from 2021 to the first quarter of 2023. During the period from January–March 2023, there was a 325% rise in defined daily dose (DDD) per 100 patient visits, compared with that in 2022. This significant rise in DDD highlights the need for further investigation into potential prescribing issues.
Hence, the authors initiated this study as part of antimicrobial stewardship (AMS) efforts to optimise azithromycin use, in line with principles aimed at reducing AMR and preventing patient harm.10 Implementing AMS programmes in the ED has been shown to improve guideline adherence in treating CAP, increasing compliance rates from 20% to 29%, reducing unnecessary antibiotic use, and promoting more appropriate prescribing.11,12
OBJECTIVES
General Objectives
To describe the prescribing practices and assess the appropriateness of oral azithromycin prescribing for the treatment of CAP in the ED of a tertiary hospital.
Specific Objectives
- To describe the clinical characteristics of patients with CAP prescribed oral azithromycin.
- To describe the dosage regimen and treatment completion for oral azithromycin in CAP.
- To assess guideline compliance with oral azithromycin prescriptions in the ED for CAP.
- To determine the clinical outcomes and factors associated with guideline compliance.
METHODS
Study Design and Setting
This was a retrospective cross-sectional study conducted in the ED of a tertiary care hospital in Malaysia.
Study Population
All patients who sought medical assistance at the ED between June 1–August 31, 2023, were reviewed. The data collection period from June–August 2023 was selected to efficiently capture prescribing patterns and related issues, following a 325% increase in the DDD of azithromycin per 100 patient visits from January–March 2023, compared with 2022. This timeframe will enable timely feedback to prescribers, help identify key concerns, and propose effective measures to address them, which will guide further work in the study.
Patients aged 18 years and older who were prescribed oral azithromycin in tablet form for the treatment of CAP were eligible for inclusion. Cases with incomplete data, azithromycin prescriptions in other forms (e.g., syrup or injectable azithromycin), patients with CAP who were not prescribed oral azithromycin, and prescriptions of azithromycin for non-CAP infections, were excluded.
Data Collection
The hospital ED registry and Pharmacy Information System (PhIS) were utilised to identify patients who visited the ED and were prescribed azithromycin tablets during the study period. The clinical notes of patients were traced and reviewed in the ED record unit. For patients who were admitted to wards, information was obtained from their inpatient case notes.
Data such as age, gender, comorbidities, diagnosis, CURB-65 score, azithromycin dosage regimen, antimicrobial exposure in the past month, concurrent antibiotics prescribed, ward admission, and continuation of azithromycin in the ward, were retrieved from ED records, inpatient clinical notes, and treatment charts by data collectors, who were pharmacists. All relevant information was recorded in an electronic data collection form.
Statistical Analysis
Descriptive analysis (percentage, frequency, median, and interquartile range) and tests for association (using Chi-square test for independence or Fisher’s exact test) were conducted using IBM Statistical Package for Social Science Software (SPSS) version 24.0 (IBM Corp., Armonk, NY, USA) to assess the relationship between guideline compliance, clinical characteristics, and outcomes. A p value of <0.05 was considered significant.
Ethical Consideration
The study was registered with the National Medical Research Register (NMRR; ID-24-00084-JTY), and ethical approval was obtained from the Medical Research and Ethics Committee (MREC) of Malaysia. Due to the observational nature of the survey, the need for informed consent was waived.
Definitions
Guideline compliance is defined as prescribing the preferred or alternative agent, route, dose, and frequency as outlined in the National Antimicrobial Guideline (NAG),13 with evaluation based on the documentation in patient records. Data collection and analysis were conducted based on NAG 2019, prior to the release of the updated NAG in July 2024. Following consultation with an infectious diseases physician, the authors decided to reassess the compliance of azithromycin prescribing, incorporating some modifications. For patients admitted to wards, irrespective of their CURB-65 score, azithromycin prescribing in the ED was assessed as guideline-adherent (Table 1).
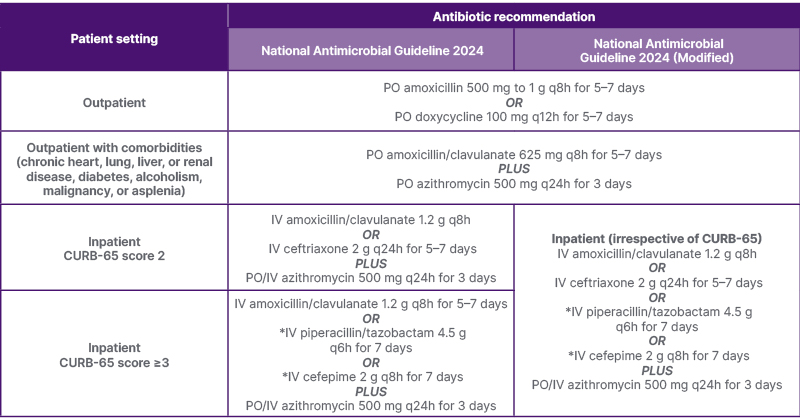
Table 1: Antibiotic recommendations for adult community-acquired pneumonia based on the National Antimicrobial Guideline 2024 and the modified version for institutional practice.
*At risk of pseudomonal infection.
IV: intravenous; PO: per oral; q8h: every 8 hours; q12h: every 12 hours; q24h: every 24 hours.
CURB-65 is a clinical prediction rule to identify patients with community-acquired pneumonia requiring hospital admission. The criteria used in the score are new-onset confusion, serum urea >7 mmol/L, respiratory rate of ≥30/min, blood pressure ≤90/60 mmHg, and age ≥65 years. Patients are stratified as follows:13
Score 0–1: Mild. Can manage as an outpatient.
Score 2: Moderate. Consider admission.
Score 3–5: Severe. Inpatient admission. Consider ICU referral.
The defined daily dose is the assumed average daily maintenance dose of a drug for its primary indication in adults. The defined daily dose for oral azithromycin is 0.3 g.14
RESULTS
Baseline Characteristics
After reviewing the medication charts of 207 patients, 165 (79.2%) fulfilled the inclusion criteria and were considered for this study. Forty-two patients were excluded for the following reasons: eight patients were <18 years of age and 34 had a non-CAP diagnosis at the time of ED presentation, including hospital-acquired pneumonia (HAP), leptospirosis, and infective diarrhoea. Of the 165 patients who received oral azithromycin, 53.3% were <65 years old, and the majority (53.3%) were female. A total of 83.6% of patients had at least one comorbidity, with hypertension being the most prevalent (63.6%), followed by diabetes mellitus (35.8%)and dyslipidaemia (31.5%).
A CURB-65 score of ≥2 was observed in 55 of the 165 patients (33.3%), meeting the criteria for hospital care of CAP. Only 10% of the patients had a documented history of antibiotic consumption in the past month. Among the hospitalised patients (71.5%), only 52 (44.1%) had a CURB-65 score of at least ≥2, while 26.3% had concurrent non-CAP diagnoses, including decompensated congestive heart failure (35.5%), fluid overload due to renal disease (12.9%), and acute coronary syndrome (9.7%). Table 2 displays the baseline characteristics of the 165 patients.
Prescribing Details
As shown in Table 2, most patients (67.9%) were prescribed a 3-day oral azithromycin course of 500 mg once daily. Three out of 10 patients were administered only a single 500 mg dose, while two patients were prescribed a 5-day regimen. Intravenous (IV) amoxicillin/clavulanate was the most frequently administered concurrent antibiotic with azithromycin (69.3%), followed by oral amoxicillin/clavulanate (27.1%), IV ceftriaxone (0.6%), and oral amoxicillin (0.6%). Four patients received no concurrent antibiotics. One patient was prescribed a single dose of IV amoxicillin/clavulanate, followed by IV ceftriaxone in the ED.
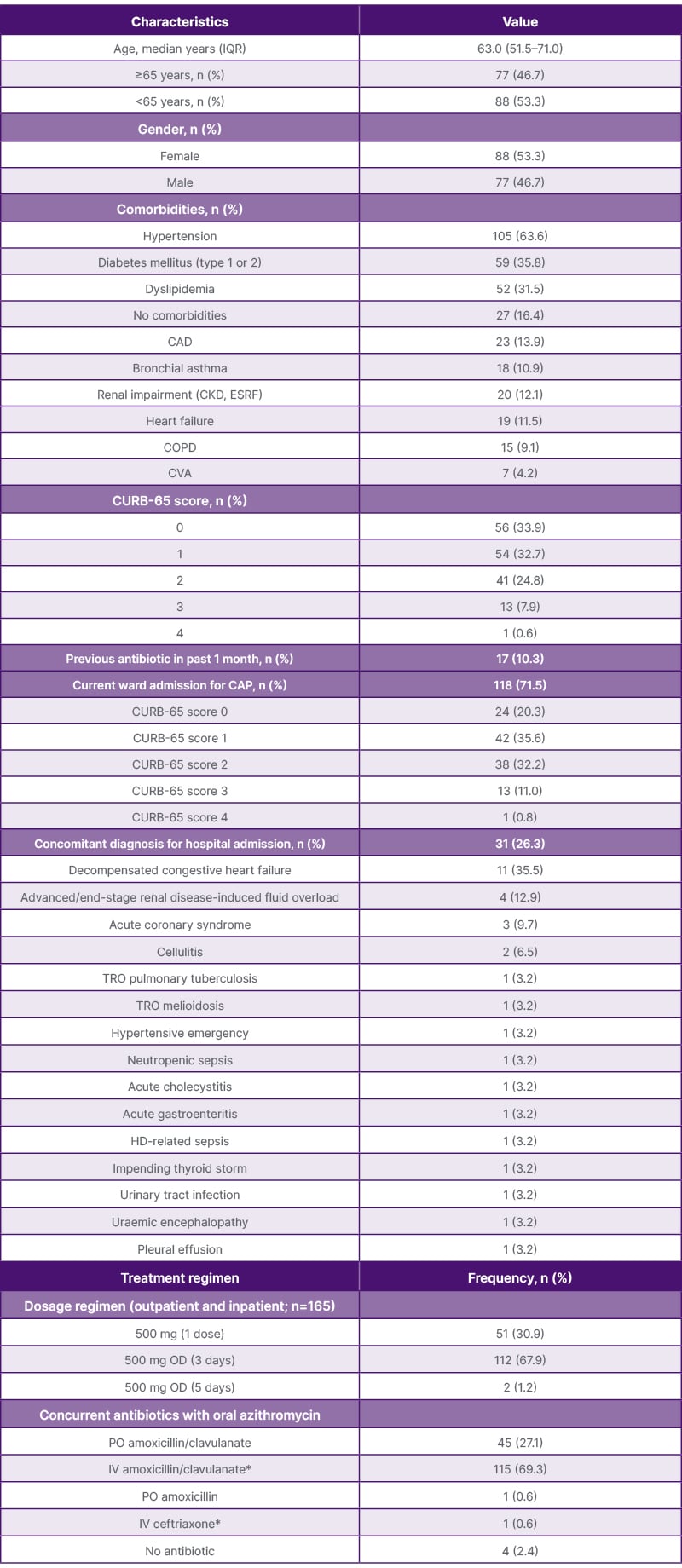
Table 2: Baseline characteristics of 165 patients and prescribing details of oral azithromycin in the emergency department to treat CAP.
CAD: coronary artery disease; CAP: community-acquired pneumonia; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; CVA: cerebrovascular accident; ESRF: end-stage renal disease; HD: haemodialysis; IQR: interquartile range; IV: intravenous; OD: once daily; PO: per oral; TRO: to rule out.
*One patient was prescribed one dose of IV amoxicillin/clavulanate, followed by one dose of IV ceftriaxone in the emergency department.
Treatment Completion
Following their admission to the ward, oral azithromycin was discontinued for 43.2% of the patients by the attending physician. The three most frequent reasons for stopping azithromycin were a CURB-65 score of <2 (21.6%), a change in the diagnosis related to the illness (17.6%), and the presence of an infection for which antibiotics were not necessary (17.6%). Additionally, 13.7% of patients required the drug to be administered via the IV route, while 15.7% had their therapy interrupted due to QTc prolongation. Other causes included antibiotic escalation (7.8%), prescriber preference (3.9%), and patient death (2.0%). These findings are outlined in Table 3. Table 4 shows no association between treatment completion or discontinuation and clinical outcomes, such as inpatient mortality.
Guideline Compliance
The majority (73.8%) of tablet azithromycin prescriptions complied with the NAG. Of the 26.2% of non-compliant prescriptions, all were due to inappropriate use of azithromycin (not the preferred or alternative option) for the outpatient treatment of patients without comorbidities, as detailed in Table 3.
In Table 4, the association between guideline compliance, patient characteristics, and outcomes is described. Tablet azithromycin prescriptions in the ED were more likely to be guideline-adherent in patients aged 65 years or older and those with comorbidities such as hypertension, renal impairment, heart failure, and COPD. As all hospitalised CAP cases were guideline-adherent, a statistical association with clinical outcomes, such as inpatient death or live discharge, could not be computed.
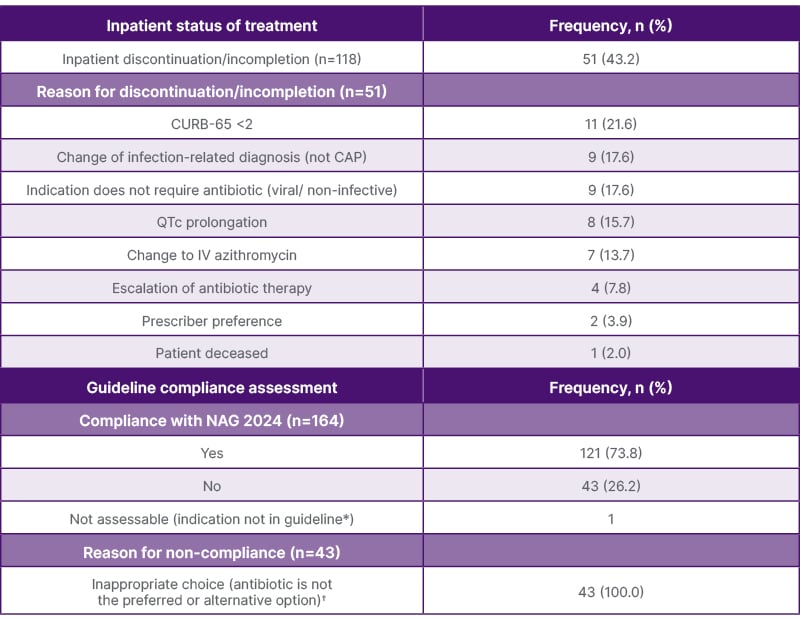
Table 3: Continuation of oral azithromycin for CAP in patients admitted to the ward (n=118) and guideline compliance.
CAP: community-acquired pneumonia; IV: intravenous; NAG: National Antimicrobial Guideline.
*One case, labeled “Not assessable due to indication not in guideline (i.e., atypical pneumonia),” will not be included in the denominator for the compliance calculation. Only 164 cases will be analysed for compliance.
†Not the preferred or alternative option for outpatient treatment in the absence of comorbidities.
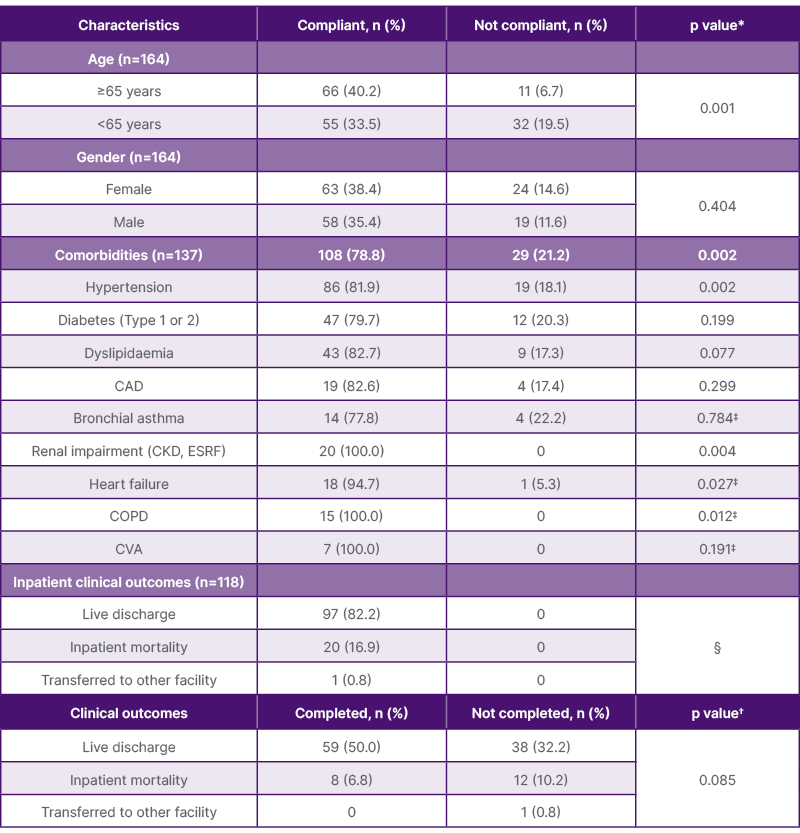
Table 4: Association of guideline compliance with patient characteristics and clinical outcomes, and inpatient tablet azithromycin treatment completion with clinical outcomes.
CAD: coronary artery disease; CKD: chronic kidney disease; CVA: cerebrovascular accident;
ESRF: end-stage renal disease.
*Chi-square test for independence, unless otherwise stated.
†Fisher–Freeman–Halton exact test.
‡Fisher’s exact test.
§Unable to compute tests for association.
DISCUSSION
The ED plays a pivotal role in managing improper antibiotic prescribing, serving as the bridge between the community and the hospital.15 This study offers valuable insights into the current practices of prescribing azithromycin tablets in the ED of a 600-bed tertiary hospital in Perak, Malaysia, for the treatment of CAP. In line with these practices, the patient demographic reveals important trends that shape antibiotic prescribing patterns.
Most patients presenting to the ED were <65 years of age, which aligns with the demographic profile of the district, where 65.2% of the population is aged between 15 and 64 years.16 A predominant comorbidity profile of diabetes mellitus and hypertension was observed, consistent with findings from a local study that indicated individuals with such conditions were more likely to receive a prescription for an antibiotic combination, including a macrolide.17 This prescribing practice follows the NAG of Malaysia, which recommends combining azithromycin with amoxicillin/clavulanate for patients with CAP and comorbidities, even in mild cases.13
In line with the NAG, this study shows that the most frequently prescribed concomitant antibiotic with azithromycin for treating CAP is amoxicillin/clavulanate. The high clinical success rate of amoxicillin/clavulanate in treating respiratory tract infections supports its use as an empirical antibiotic.18 Although it is listed as an alternative antibiotic for CAP in local guidelines, third-generation cephalosporins, such as ceftriaxone, were rarely encountered during the study period. This contrasts with another local study that reported ceftriaxone was combined with azithromycin in approximately 10% of prescriptions for both non-severe and severe pneumonia in patients with comorbidities.17
In the management of CAP, CURB-65 is a preferred severity prediction score, as all the parameters needed to compute the score are easily accessible.19 A score of at least 2 indicates moderate-to-severe pneumonia and suggests consideration for hospital admission. One limitation of the CURB-65 approach is that it does not consider comorbid conditions, which may restrict its applicability for patients who encounter a high mortality risk if even a mild case of CAP exacerbates a chronic, but stable disease.20 In this study, more than 50% of hospitalised patients with azithromycin had a CURB-65 score of <2, suggesting mild CAP. This finding is consistent with a study conducted in Australia, where 64% of hospitalised patients received azithromycin despite not meeting the CURB-65 criteria.19 Additionally, therapy discontinuation was observed in this cohort, with only 56.8% of patients continuing azithromycin in the ward, compared to 80.2% in a previous study that examined ED-prescribed antibiotics maintained through discharge.21
While these findings shed light on prescribing practices, patient safety remains a key consideration, particularly regarding the potential adverse effects of macrolide antibiotics like azithromycin. One recognised risk is QTc interval prolongation, which can lead to sudden cardiac death and lethal arrhythmias.22,23 In this study, 7% of hospitalised patients experienced this adverse event, detected through routine ECGs, an assessment not performed in the outpatient ED setting. Many patients in this cohort had significant cardiovascular risk factors, such as hypertension, diabetes, and dyslipidaemia. Given its proarrhythmic effects, azithromycin has been associated with increased cardiovascular mortality, especially among those with a high baseline risk of cardiovascular disease.24
In addition to these safety concerns, the choice of administration route for azithromycin is an important factor in optimising treatment for CAP. In this study, 6% of patients required conversion from oral to IV azithromycin due to inadequate gastrointestinal absorption of oral antibiotics in critically ill individuals. Considering this, patients hospitalised for CAP, especially in severe cases, typically begin therapy via the IV route.25 Nonetheless, data indicate that the effectiveness of orally administered azithromycin is equivalent to that of IV administration, and one study also showed elevated concentrations of azithromycin in lung tissues following oral administration.25,26 Oral azithromycin is also much less expensive and reduces the risks associated with IV medication administration, such as thrombophlebitis and infection.27
Several studies have evaluated the rates of appropriate antimicrobial prescribing in the ED, comparing compliance against national or institutional antimicrobial guidelines. The lowest compliance rate reported was 19.1%, while one study reported the highest rate at 76.0%.28,29 In the ED of a tertiary hospital in Malaysia, the overall compliance rate was 46.9%.30 Other studies reported rates ranging from 32.5–62.0%.31–34 Reasons for non-adherence to guidelines included duration (28.6%), not indicated or not a bacterial infection (15.2%), choice of therapy (34.3–53.4%), dosing (10.3–21.9%), or both choice of therapy and dosing (36.2%).31,32
While many studies have evaluated compliance with empirical antimicrobial guidelines for managing hospitalised patients with CAP, such data remain scarce in the ED setting. Available evidence shows that these rates vary across studies in the treatment of lower respiratory tract infections, including CAP. Bauman et al.29 observed the highest compliance rate among the studies reviewed at 95.0%, while Robinson et al.35 reported the lowest at 6.9%. Guideline compliance rates from other studies ranged from 28.3% to 66.3%.21,28,31,32,34,36,37 Reasons for non-compliance included inappropriate choice (26.9%) and not being indicated (65.4%).32
Evaluating the prescribing practice of a single antimicrobial agent for treating a specific infection, such as oral azithromycin, is even more uncommon. A review of current empiric prescribing practices in one ED found 25 inappropriate oral azithromycin prescriptions, with 48% deemed non-compliant due to choice, while 52% were considered not indicated.32 A retrospective chart review of patients discharged from the ED with oral antibiotic prescriptions reported that 11% or 10 patients received inappropriate azithromycin prescriptions.29
These findings highlight the need to better understand factors influencing adherence to antibiotic guidelines. A national audit of EDs in France found that the presence of COPD, congestive heart failure, and age >65 years were significantly linked to better adherence to guidelines.36 In contrast to our findings, one study indicated that patients <18 years old were more likely to receive appropriate antibiotics compared to adults (77.1% versus 63.1%).32 Additionally, another study found that non-compliance with guidelines was notably higher among males (87.1%).28
Despite these observations, there is a lack of research investigating the clinical or microbiological outcomes of guideline adherence in the ED context. A recent meta-analysis of hospitalised patients with CAP found that guideline-concordant therapy was associated with a statistically significant reduction in both 30-day and in-hospital mortality rates. However, due to significant heterogeneity, the effect of guideline adherence on length of stay, ICU admission, re-admission rates, clinical cure, and adverse effects was not evaluated.38
Given these gaps, the findings of this study indicate that the ED represents a critical setting for initiating AMS interventions aimed at reducing inappropriate prescribing. A multifaceted approach is recommended, combining educational interventions for ED staff and the implementation of standardised clinical pathways and guidelines.15 These protocols should be easily accessible, tailored to factors such as patient age, comorbidities, and disease severity, and designed to guide prescribing practices, ensuring consistency and reducing variability in antibiotic use. Educational interventions should focus on the importance of adhering to national antimicrobial guidelines, recognising the risks of AMR, and identifying when antibiotics are unnecessary. Regular antimicrobial audits followed by feedback can identify areas where prescribing deviates from guidelines and provide opportunities for improvement.15
Previous studies have shown that multifaceted educational interventions for treating CAP in the ED improved antibiotic concordance with guidelines from 20% to 29%.11 Investigators found that implementing guidelines and clinical pathways for respiratory tract infections can significantly change antibiotic prescription trends. When supplemented with educational activities, prescriptions of amoxicillin/clavulanate and cefpodoxime were reduced from 43.0% to 10.2% and from 16.6% to 2.5%, respectively, with a complementary rise in amoxicillin prescriptions from 34.0% to 84.7%.12
Limitations
As this study is retrospective, some data on confounders may be missing, unavailable, or under-investigated, leading to potential bias. Variables that could impact outcomes, such as baseline ECG, previous antibiotic regimens, chest X-rays, culture and sensitivity results, and drug allergies, may not have been recorded. It was not possible to ascertain whether antibiotics that differed from the guidelines were selected for specific reasons, unless explicitly documented.
Other limitations include the lack of formal validation of the CURB-65 scoring process and inter-rater reliability assessment across all reviewers. Additionally, the panel assessing antibiotic appropriateness and guideline compliance, which consisted of pharmacists, lacked input from a physician or infectious disease specialist, potentially limiting insights. To minimise discrepancies, discussions were held to guide decision-making in more complex cases. Azithromycin prescriptions may have varied according to patients’ risk profiles, and the exact reasons for discontinuation or failure to prescribe the drug may not have been recorded, leading to potential prescription bias. However, as this study included all patients prescribed azithromycin for CAP, and data were retrieved from records, selection and recall bias were minimised.39
Further Work
Future research should explore the impact of guideline adherence on clinical outcomes, examine the link between prescribing practices and AMR, and implement AMS measures to improve ED prescribing. Expanding the study to include comparative data across different EDs could provide further insights.
CONCLUSION
In summary, the compliance of oral azithromycin prescribing with national guidelines for CAP in the ED of this tertiary hospital was moderate. There is a need to extend AMS interventions to the ED to ensure that the most appropriate empiric treatment is initiated for CAP and other infections.







