Meeting Summary
In August 2025, EMJ conducted individual interviews with two European medical experts and a patient advocate who had survived infection in adolescence on the critical importance of timely immunisation against invasive meningococcal disease (IMD) in adolescents. The discussions highlighted the disease burden, lasting sequelae, and the global need for improved vaccine coverage, particularly against serogroup B (MenB), the leading cause of IMD in Europe. The interviews underscored a second peak of IMD incidence in adolescence and the challenges in integrating MenB and MenACWY vaccines into national immunisation schedules, which currently results in suboptimal vaccine uptake in this age group. This article aims to shed light on the need and opportunities to help protect adolescents against IMD.WHY DOCTORS, NURSES, AND PARENTS CARE ABOUT INVASIVE MENINGOCOCCAL DISEASE
IMD is an uncommon and unpredictable disease with a high case fatality rate.1 Five to ten percent of patients with IMD die within the first 48 hours, with the majority being children and young people, and 10–20% of survivors experiencelong-term sequelae.2
Kate, an advocate for meningitis awareness, is one of those survivors. Her IMD with septicaemia at the age of 16 years left her with scarring as well as non-visible sequelae. “I went from thinking I had a minor illness to being in critical condition within a matter of hours,” Kate explained to EMJ.
“Recovery took a really long time to regain my strength. I missed months of school, I dealt with surgeries, wound care, physiotherapy, and numerousspecialist appointments.”
Meningococcal disease rates vary with age, with the highest rates typically observed among infants, but a second, smaller peak in incidence occurs in adolescents and young adults (Figure 1).3-5 Rivero-Calle, Consultant in Paediatrics and Paediatric Infectious Diseases, Translational Paediatrics and Infectious Diseases Section, Hospital Clínico Universitario de Santiago de Compostela, Galicia, Spain, points to epidemiology trends of serogroup B causing the majority of IMD cases in Europe.3,4,6
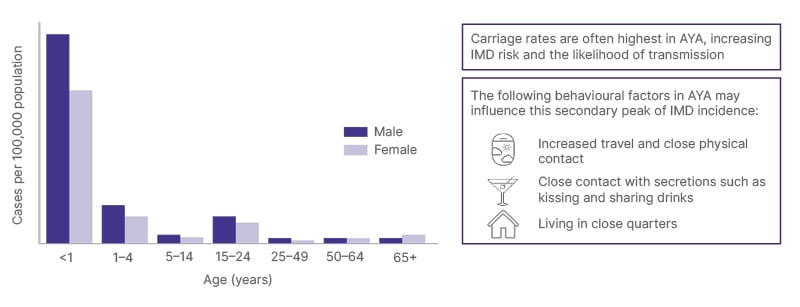
Figure 1: Distribution of confirmed IMD cases per 100,000 population by age and gender, EU/EEA, 2022.
Source country reports from Austria, Belgium, Bulgaria, Croatia, Cyprus, Czechia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Liechtenstein, Lithuania, Luxembourg, Malta, the
Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Spain, and Sweden.
Adapted from ECDC table titled ‘Distribution of Confirmed IMD Cases per 100,000 Population by Age and Gender, EU/EEA, 2022′.5
AYA: adolescents and young adults; EEA: European Economic Area; IMD: invasive meningococcal disease.
THE AT-RISK AGE GROUP THAT COULD FALL THROUGH THE CRACKS OF PAEDIATRIC CARE
“Meningitis can affect anyone, no matter what age group,” emphasised Rivero-Calle in her interview with EMJ.
In the USA, MenB has been reported to account for 56% of meningococcal disease cases in children and young adults aged 11–23 years.3 Last year, Spain saw the same number of meningococcal disease cases among patients aged 10–14 years as occurred in older adolescents aged 15–19 years, 7 according to Rivero-Calle.
Adolescents face increased IMD risk and likelihood of transmission, in part because of ‘sharing’ behaviours such as cigarettes or vaping, and crowded living conditions associated with summer camps and communal housing.3,4
Carriage of one type of meningococcal bacteria (Neisseria meningitidis) in the nasopharynx has been shown to peak at around 23.7% in adolescence, making this age group a potential reservoir and transmitter of the disease.8 Moreover, tobacco has been linked to an increased risk of IMD by increasing nasopharyngeal colonisation, even in passive smokers.9
Despite incidence data and age-related risk, both medical experts interviewed for this article agree that adolescent patients often miss the opportunity to be vaccinated, particularly against the most common disease-causing serogroup in Europe, Meningococcus B.3,4,6
In countries where adolescent-aged patients are typically still under the care of paediatricians, this missed opportunity could be corrected, according to Gabutti, Member of the Vaccines and Vaccination Policies Working Group of the Italian Scientific Society of Hygiene, Preventive Medicine and Public Health, Italy. “Adolescence is a critical age, where we can administer boosters to those who were immunised as infants and reinforce the immunological response…and also locate those who are vaccine naïve and provide full immunisation.” Healthcare professionals (HCP) have a large role to play, he says, in part because adolescents themselves may lack awareness of the disease, its serogroups, or any protection options.
THE LASTING EFFECT OF INVASIVE MENINGOCOCCAL DISEASE SEQUELAE
Kate contracted IMD at summer camp in Nova Scotia, Canada, at the age of 16 years. She explained that through her patient advocacy, she has gained a first-hand insight into the breadth and severity of disease sequelae. “The sequelae are so numerous and so varied, the effects of this disease take their toll, and it is heavy.”
One in five survivors of bacterial meningitis experiences long-term sequelae, including hearing loss; impaired vision, speech, language, memory, and communication; seizures; paraparesis; scarring deformities; and limb amputations.2
Rivero-Calle noted that in her experience, adolescents tend to seek medical care later on in the disease course. This experience corresponds to findings that the median time from onset to hospital admission was longer in adolescents (22 hours in those aged 15–16 years) compared with younger children (13–14 hours in those aged <1–4 years).10 Rivero-Calle attributed this discrepancy, particularly in adolescents, to the non-specificity of some symptoms such as abdominal pain or vomiting.
For Kate, after initially falling sick at a rural summer camp, she was taken to a nearby hospital, where a broad-spectrum antibiotic was administered. When her condition did not improve, she was transferred to a larger hospital. “In that ambulance is where I got the sore neck and headache…which are the telltale signs.” By the time Kate had arrived at the second hospital, clinicians were able to perform a spinal tap to confirm IMD.11 Then, Kate was put in an air ambulance and travelled to a third hospital which was 4 hours away. Here, she was put into a medically induced coma, spending a week in the ICU and another 3 weeks in the hospital after that. She added: “The doctors said I had a 5% chance of making it through the night.” In the longer term, Kate shared that she had to relearn how to walk, regaining strength in her body whilst feeling constantly fatigued. “People thought that because I was young, I would bounce back quickly… but that wasn’t the case; it took months to regain some normalcy in my life.”
Highlighting data from Europe, Rivero-Calle explained that delays in disease recognition among adolescents lead to more complex and costly long-term sequelae compared to those in infants.3 Additionally, compared with age- and sex-matched controls, adolescent survivors of IMD reported a reduction in quality of life, including fatigue, decreased social support and educational outcomes, as well as deficits in memory, attention, and psychomotor speed.10 Individuals who contracted IMD as younger adolescents also showed a greater degree of cognitive deficit compared to those who contracted IMD later in adolescence.11
EXISTING, BUT UNDER-UTILISED PREVENTION TOOLS
There are efficacious vaccines that can help protect adolescents against five of the six leading IMD-causing serogroups,3 including single serogroup vaccines for serogroups A, C, and B. Combination conjugate vaccines for conjugate MenACWY are included in adolescent programmes of 30 countries and pentavalent MenABCWY has recently been authorised in the USA.3
Vaccines specifically against MenB, the most prevalent disease-causing serogroup in adolescents and young adults, are included in far fewer national adolescent vaccination programmes than vaccines for other serogroups, like conjugate MenACWY, and uptake and series completion is far from optimal (Table 1).
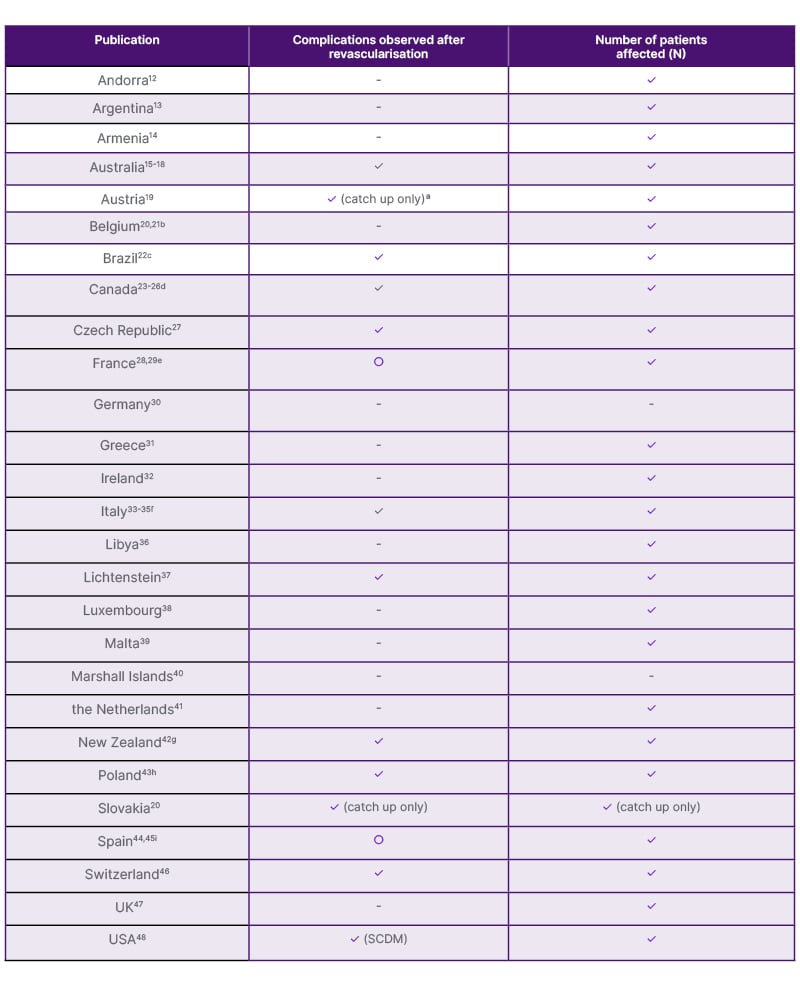
Table 1: Current adolescent Meningococcal serogroup vaccination recommendations. (GSK, Data on File)
✓ Fully included in NIP
✓Medical professional society recommendation only
○ Recommended; not in NIP/RIP – Not available
aCatch-up recommended, but not free of charge.29
bNot funded by the National Health System.20
cIf MenACWY is not available, MenC can be used. MenB is only available through private vaccination clinics.22
dMenC or MenACWY vaccine chosen depends on local epidemiology and programmatic considerations.23
eMenB available on basis of HCP recommendation for all AYA aged 15–24 years.28
fMenB integrated in regional programmes.
gAYA aged 13–25 years who will be living or are currently living in a boarding school hostel or university hall of residence, military barracks, youth justice residences or prison, including those who turn 13 years of age while living in a boarding school hostel.42
hAlthough in the NIP, MenB and MenACWY are recommended rather than mandatory, and not funded. Vaccinations are free of charge from 9–14 years of age and reimbursement is available for one vaccine from 9–18 years of age.43
iMenB recommended for AYA by national paediatric association.46
AYA: adolescents and young adults; HCP: healthcare professional; Men B/C/ACWY: meningococcal serogroup B/C/ACWY; NIP: National Immunisation Programme; RIP: Regional Immunisation Programme; SCDM: shared clinical decision-making.
OPTIMISING VACCINATION SCHEDULES: ADVICE FROM THE EXPERTS
Adolescent vaccination schedules for IMD protection also vary between countries. For example, in New Zealand and Canada, conjugate MenACWY vaccination is recommended when adolescents begin living in close quarters, such as military recruits or higher education students.23,42 Other countries, such as Switzerland and Australia, recommend conjugate MenACWY administration in early adolescence and offer catch-up vaccinations intoearly adulthood.15,46
Rivero-Calle emphasised the importance of scheduled vaccination appointments to maximise vaccine uptake. For example, integrating vaccinations into pre-existing appointments: “In early adolescence, there is often a scheduled visit in child and adolescent care programmes, so a new specific vaccination appointment would not be needed.”
Both experts agreed that, if possible, HCPs should aim to immunise adolescents whilst they remain under paediatric care, before entering adult care. Gabutti reflected that in early adolescence, childhood-primed patients can benefit from a booster dose (MenB vaccines are not interchangeable, and boosters should be done with the same vaccine previously administered), and those who are vaccine-naïve can be immunised before leaving paediatric care.
By co-administering conjugate MenACWY and MenB vaccines, the experts agreed that the message of prevention against IMD is strengthened across all serogroups.
“Each country has a different approach,” Rivero-Calle stated. “We must think practically about the possibility of administration, using any chance we can take to immunise. Some countries offer boosters alongside [human papillomavirus] HPV, or [tetanus and diphtheria] TD. What we need is a balance between maintaining immune response and protecting those who are vaccine naïve.”
TIPS ON TIMING
Kate, Giovanni, and Rivero-Calle all agreed that to tackle the second peak, there is no single ‘best time’ to treat adolescents. Instead, multiple points during adolescence are suitable for IMD prevention and depend on country-wide vaccination scheduling, as well as practical and organisational aspects.
For example, administering vaccinations while patients are still school-age helps younger adolescents gain protection ahead of the second peak, Rivero-Calle and Gabutti explained, although noting the duration of protection data for MenB vaccines is still evolving and protection may wane before college age. Understanding both the immune persistence of a MenB (the sustained circulation of antibodies produced in response to vaccination) and its duration of protection (the length of time after vaccination when the vaccine can be effective in preventing disease) helps her advise patients and vaccinate at anoptimal time.
With 4CMenB, immune persistence has been observed up to 7.5 years after adolescent vaccination, while a study in South Australia, which showed no 4CMenB effect on carriage of disease-causing meningococci,49 has demonstrated high protection against MenB disease in adolescents after 5 years.50-52
Whilst experts agreed that the scheduling of adolescent vaccinations at a set age is best for ensuring series completion, Rivero-Calle says HCPs need to remain flexible. A patient may need customised scheduling, due to reasons such as travel needs.
All three experts underscored the importance of accessibility to vaccines and effective education surrounding them. Gabutti recommends thinking beyond the paediatrician’s office, suggesting vaccine drives in public places such as schools. He highlights the potential role of general practitioners in supporting and administering this vaccination.
Kate agrees, saying paediatricians can be proactive and help teens and pre-teens plan for vaccination opportunities. “Find key steps in an adolescent’s life, like going to summer camp or leaving school and going to university, where teenagers will be spending time away from home and taking their life into their hands for the first time.”
ANOTHER TOOL TO HELP HEALTHCARE PROFESSIONALS DETERMINE WHEN TO VACCINATE: SURVEILLANCE DATA
Rivero-Calle and Gabutti both prioritise local epidemiological and surveillance data to inform decision-making around when to vaccinate and recommend this approach for HCPs in countries without national immunisation programmes. They encourage peers to consider the local incidence of meningococcal disease, age distribution of cases, and any identified risk groups of focus. In their respective countries, Italy and Spain, surveillance guidance tracks disease distribution, genetic characterisation, and any vaccine failures.53,7 Gabutti emphasised that surveillance data can aid the development and rollout of vaccination campaigns.
“Surveillance is useful to understand and have a precise knowledge of what is going on,” Gabutti said. “And more importantly, that we stay up to date on this data and work as a team.” Moreover, HCPs need to know which type of surveillance system is in place. Routine, active surveillance provides comprehensive and timely data, while passive surveillance (relying on reports of cases) may underestimate the true burden.
He also recommended taking a general approach based on epidemiology and immunology rather than focusing exclusively on risk. For example, if an adolescent does not plan to attend college or university, this does not mean they would not benefit from vaccination. Their age group still puts them at risk. This is where he said a defined age range for vaccination is useful.
Gabutti highlighted how IMD outbreaks in the USA have provided important lessons for the optimisation of vaccination coverage. A spate of college-related IMD outbreaks in the USA underscored the importance of timeliness in vaccination and the vulnerability of adolescents in close-contact settings. He said this has driven greater public awareness and proactive prevention; the USA approach builds on MenC/ACWY programmes and offers MenB vaccination later in adolescence.48
ADDRESSING THE INVASIVE MENINGOCOCCAL DISEASE KNOWLEDGE GAP AT ADOLESCENCE
Kate says that before contracting IMD, she had little knowledge about the disease or that it could affect adolescents instead of just infants and young children. “I had heard about outbreaks on the news but never thought it would happen to me. You’re 16. You’re invincible.”
Gabutti echoes Kate’s point, expressing that in his experience, whilst HCPs possess robust knowledge of IMD, their primary challenge lies in translating knowledge into consistent, practical strategies and communication driving vaccine uptake in adolescents andtheir families.
Not insurmountable, says patient Kate. Paediatricians should talk directly to the adolescent in the room, so they feel engaged in an inclusive conversation. “It’s just as simple as doctors making eye contact while they’re talking with adolescents instead of just to the adult. Especially when children grow into adolescence, they won’t see the doctor as much, so it is important they do, and are included in conversation.”
Rivero-Calle echoes this, encouraging HCPs to “explain the reality of the possible outcomes of the disease, even show them pictures of how devastating it can be…in this era with all its internet platforms, we can even show blogs and websites of adolescent patients, survivors of IMD.”
Kate advises providing adolescents with clarity on their own decision-making, focusing on opportunities to prevent disease. “When the foundations are put in younger, these teenagers will come into themselves, growing up into fully informed adults, able to take control of themselves and understand the implications of the interactions they may have with their peers.”
“Prevention and education are key. Take the time to talk to your patients, know what their doubts are, solve misconceptions, and provide evidence-based answers to common questions both for the public and HCPs, and thereby assist individuals in making healthy choices for themselves and their families,” summarised Rivero-Calle.
“Vaccines only work if they are used, and it is our responsibility as HCPs to be trained, to inform our patients and to help reduce vaccine-preventable IMD deaths and suffering as much as possible. Don’t lose any opportunity to do so!”
In conclusion, Rivero-Calle, Gabutti, and Kate hope HCPs use evidence-based approaches to support IMD prevention at any point in adolescence, including disease caused by serogroup B. As Rivero-Calle put it: “The only non-optimal age to recommend vaccination is after an adolescent contracts IMD.”
| Adverse events should be reported. Reporting forms and information can be found at: https://yellowcard.mhra.gov.uk/ (UK) or search for MHRA Yellow Card in the Google Play or Apple App Store. Adverse events should also be reported to GSK: please call 0800 221 441 or email [email protected] |







