BACKGROUND AND AIMS
Chronic kidney disease (CKD) is a global public health problem with a high impact on morbidity and mortality.1 Diabetes is one of the leading causes of CKD, and up to 40% of patients with Type 2 diabetes (T2D) have CKD.2 Although patients with metabolic diseases are primarily managed by endocrinology units, there are currently no studies describing the burden associated with the loss of kidney function and the risk of developing hyperkalaemia in these patients. The ENDO-CKD study aimed to describe and characterise the prevalence, associated burden, and management of hyperkalaemia in patients with T2D and CKD managed by endocrinologists in Spain.3
METHODS
This was a retrospective observational study using data from the TELOTRON database in Spain. Adult patients with T2D (as per diagnosis code, at least one HbA1c value of ≥6.5%, or prescription of any antidiabetic drug) and CKD (as per diagnosis code or lab criteria for CKD diagnosis [one estimated glomerular filtration rate of <60 mL/min/1.73 m2 and/or one urine albumin-to-creatinine ratio of ≥30 mg/g]) with at least one visit to the endocrinology services between January 2013–November 2023 were included. Hyperkalaemia was defined as per diagnosis code and/or with potassium laboratory values >5 mmol/L. Baseline characteristics, treatments, and hyperkalaemia management were analysed.
RESULTS
A total of 8,017 patients were identified. The mean age was 70.7 years (SD: 11.8 years), 45.2% were female, the mean BMI was 31.8 kg/m² (SD: 6.5), the mean estimated glomerular filtration rate was 61.9 mL/min/1.73 m² (SD: 24.6), the median urine albumin-to-creatinine ratio was 53.5 mg/g (interquartile range: 25.0–146.2), and the median Charlson Comorbidity Index (CCI) score was 4.0 (interquartile range: 2.0–5.0). These patients were highly comorbid (81.6% hypertension; 77.8% hyperlipidaemia; 45.6% obesity; 21.4% heart failure) and had a high use of drugs (96.1% glucose-lowering; 83.5% lipid-lowering; 80.6% renin–angiotensin–aldosterone system inhibitors; 63.7% sodium-glucose cotransporter v2 (SGLT2) inhibitors; 43.1% β-blockers). Among them, 26.4% (2,116) had an event of hyperkalaemia, yet only 29.7% (628) were formally diagnosed and 12.6% (267) received treatment with potassium binders (Table 1).
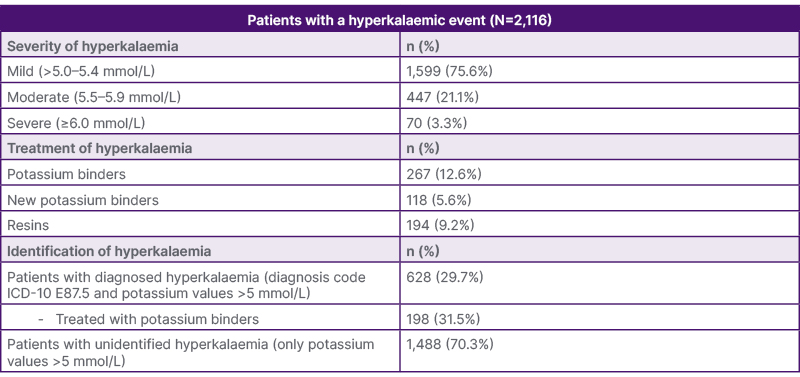
Table 1: Management of hyperkalaemia in patients with Type 2 diabetes and chronic kidney disease managed by endocrinology services in Spain.
ICD-10: International Classification of Diseases, Tenth Revision
CONCLUSION
Hyperkalaemia is a prevalent condition, but it remains underdiagnosed and undertreated in patients with CKD and T2D managed by Spanish endocrinology services, despite guideline recommendations for achieving optimal cardio-renal-metabolic therapy. Over 70% of hyperkalaemia cases are not formally identified, and more than 85% of patients do not receive appropriate treatment. The authors’ findings underscore the need for early detection and management of hyperkalaemia in high-risk patients.






