Abstract
A variety of imaging modalities, including magnetic resonance angiography, computed tomographic angiography, digital subtraction angiography, and ultrasound, can be employed to identify haemodynamic changes in patients with cerebrovascular disorders. This article underscores the diagnostic utility of neurosonological assessment of cerebral vessels through two illustrative clinical cases involving pathologies of the vertebrobasilar circulation.
Key Points
1. This article demonstrates the value of neurosonology as a non-invasive, bedside diagnostic tool through two distinct vertebrobasilar cases, one ischaemic stroke with complex haemodynamic compensation and one malformative arteriovenous fistula with reversed flow patterns, highlighting how neurosonological insights complement neuroradiological imaging and guide diagnosis, treatment planning, and follow-up.2. Neurosonology enables the dynamic, real-time evaluation of cerebral circulation, even in anatomically challenging regions such as the vertebrobasilar system. It facilitates the detection of reversed flow, collateral pathways, and velocity changes, thereby supporting risk stratification, treatment decisions, and follow-up in patients with posterior circulation disorders.
3. The accuracy and clinical utility of neurosonological assessments critically depend on the operator’s expertise, underscoring the importance of dedicated educational programmes and continuous skill development.
INTRODUCTION
Neurosonology is a versatile, non-invasive diagnostic modality for evaluating cerebral circulatory disorders.1 It provides real-time haemodynamic and morphological information, enabling the identification of occlusions, stenoses, and other vascular abnormalities. In addition to diagnostic applications, neurosonology allows for longitudinal monitoring and contributes prognostically to clinical decision-making.2 Although its morphological detail and panoramic view may be more limited compared with neuroradiological techniques,3,4 neurosonology offers distinct advantages: it is more accessible, non-invasive, easily repeatable, and can be performed without moving the patient, particularly in the stroke unit. Moreover, unlike computed tomographic angiography (CTA), it does not involve exposure to ionising radiation, and unlike magnetic resonance angiography, it can be used in patients with metallic implants or poor compliance. As such, neurosonology serves as a valuable complement to neuroradiological investigations.5,6 This article presents two clinical cases in which the combined use of neurosonology and radiological imaging facilitated a comprehensive understanding of two distinct vertebrobasilar pathologies, one ischaemic, and the other malformative.
METHODS
Neurosonological assessment was performed according to established protocols, employing extracranial and transcranial colour-coded duplex sonography for haemodynamic evaluation of the vertebrobasilar system.7 Severe intracranial vertebral artery (VA) stenosis was defined according to the criteria proposed by Danyel et al.,8 which identify a peak systolic velocity (PSV) of ≥120 cm/s in the V4 segment, together with post-stenotic flow alterations and/or collateral circulation, as indicative of high-grade stenosis (70–99%).
Whenever possible, neurosonological findings included the reporting of quantitative parameters for each evaluated vessel, specifically PSV, end-diastolic velocity (EDV), resistance index (RI), and, where appropriate, pulsatility index (PI). The RI was calculated as (PSV–EDV)/PSV, while PI was calculated as (PSV–EDV)/mean flow velocity.
FIRST CASE
A 57-year-old man presented with a 3-week history of subjective dizziness, nausea, and postural instability, with a tendency to fall to the left and difficulty walking (post-National Institutes of Health Stroke Scale [NIHSS] score of 5). The patient had a history of arterial hypertension and uncontrolled diabetes. An emergency brain CT scan showed signs of subacute left cerebellar and occipital ischaemia. As there were no indications for revascularisation treatment, the emergency study was not completed with a CTA. In the stroke unit, a comprehensive neurosonological examination of the cerebrovascular arteries revealed the following findings.
On the left side:
Patency of the VA in the extracranial segment, with a marked increase in RI (PSV: 30 cm/s; EDV: 4 cm/s; RI: 0.86; Figure 1A).
No detectable flow signal in the V3 segment, with reversed flow in the V4 segment, continuous with the ipsilateral posterior inferior cerebellar artery (PICA; PSV: 36 cm/s; EDV: 16 cm/s; PI: 0.88; Figure 1B).
On the right side:
Severe stenosis in the V4 segment (PSV: 410 cm/s; EDV: 218 cm/s; PI: 0.68; Figure 1C).
Patency of the basilar artery (BA) with a normal velocity profile (PSV: 48 cm/s; EDV: 22 cm/s; PI: 0.85; Figure 1D).
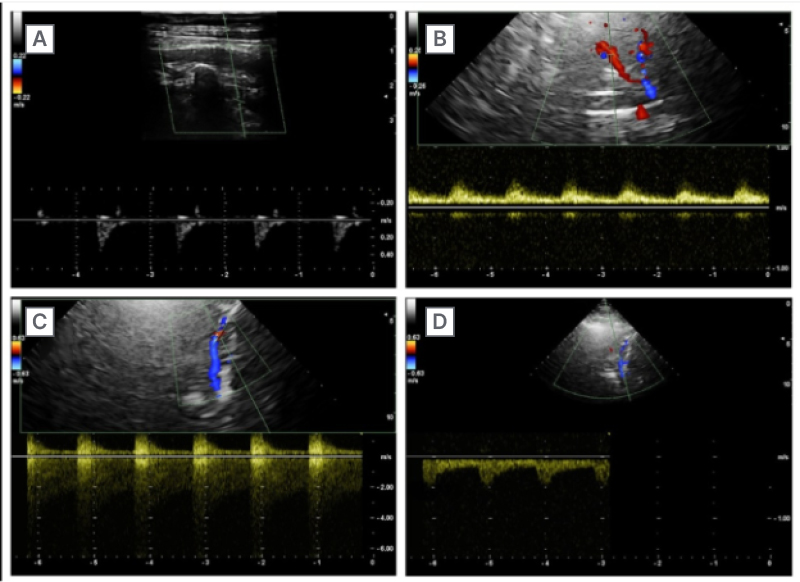
Figure 1: Neurosonological findings in Case 1 (ischaemic vertebrobasilar disease).
A) Extracranial duplex ultrasound of the left VA showing preserved patency with a marked increase in resistance index.
B) TCCD of the left V4 segment demonstrating reversed flow towards the PICA, with absent flow signal in the V3 segment.
C) TCCD of the right V4 segment showing severe stenosis.
D) TCCD of the BA revealing normal flow velocity profile and direction.
BA: basilar artery; PICA: posterior inferior cerebellar artery; TCCD: transcranial colour-coded Doppler; VA: vertebral artery.
Subsequent CTA confirmed severe stenosis in the right V4 segment, normal visualisation of the left VA from its origin to the distal V2 segment, missing V3 segment, and reappearance in the V4 segment before terminating in the PICA (Figure 2). The case was discussed with interventional radiology and, given the patient’s asymptomatic status and adequate haemodynamic compensation, the best medical treatment was chosen. This included dual antiplatelet therapy (aspirin 100 mg daily and clopidogrel 75 mg daily) and atorvastatin 80 mg daily for 3 months, followed by clopidogrel 75 mg daily and atorvastatin 40 mg daily.
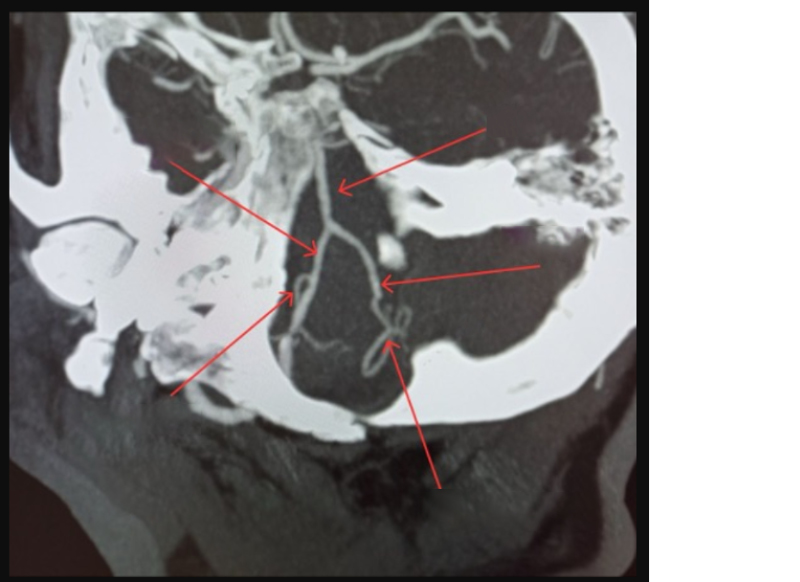
Figure 2: Computed tomographic angiography findings in Case 1.
CTA confirming severe stenosis of the right V4 segment. The left VA is visualised from its origin to the distal V2 segment, with absence of opacification in V3 and reappearance in V4 ending in the PICA, consistent with segmental occlusion and distal re-entry.
BA: basilar artery; CTA: computed tomographic angiography; PICA: posterior inferior cerebellar artery; VA: vertebral artery.
The patient continues to undergo neurosonological follow-up. Angiographic intervention with potential stent placement remains a secondary option in the event of clinical deterioration. In this clinical setting, serial neurosonological evaluation remains an indispensable tool for haemodynamic surveillance, achieved by 1) quantifying the post stenotic peak systolic velocity in the right V4 segment, a surrogate of satisfactory inflow to the left posterior inferior cerebellar artery through the inverted ipsilateral vertebral artery and, by extension, to the basilar trunk; and 2) ascertaining the direction of flow within the basilar artery, which, when orthograde, confirms adequate perfusion from the stenotic V4 vertebral artery, but when retrograde it indicates the recruitment of carotid–posterior communicating collateral pathways. Non-invasive monitoring not only provides essential insights into haemodynamics, but also supports therapeutic decision-making regarding the timing of potential endovascular intervention.
SECOND CASE
An 11-year-old girl presented with a palpable, pulsatile swelling in the right suboccipital region. A previously performed magnetic resonance angiography revealed malformed vessels in the right lateral cervical region, involving the jugular bulb and the extracranial segment of the ipsilateral VA, with venous structures pertaining to the external jugular vein and the vertebral vein in a pattern suggestive of an arteriovenous fistula or malformation.
The neurosonological examination revealed:
Enlarged right extracranial VA (7.1 mm diameter) with high flow velocities and reduced RI (PSV: 190 cm/s; EDV: 90 cm/s; RI: 0.60; Figure 3A).
The right V3 segment, consisting of abnormal, convoluted arterial vessels with high flow velocities (PSV: 460 cm/s; EDV: 300 cm/s) and a PI below normal (0.2; Figure 3B), receiving inflow not only from the right V2 segment, but also from the ipsilateral V4 segment, which exhibited reversed flow, indicating a vascular steal phenomenon directed towards V3 instead of towards the BA.
Venous efferent vessels with arterialised flow draining into the internal jugular vein and the ipsilateral vertebral venous plexus (Figure 3C).
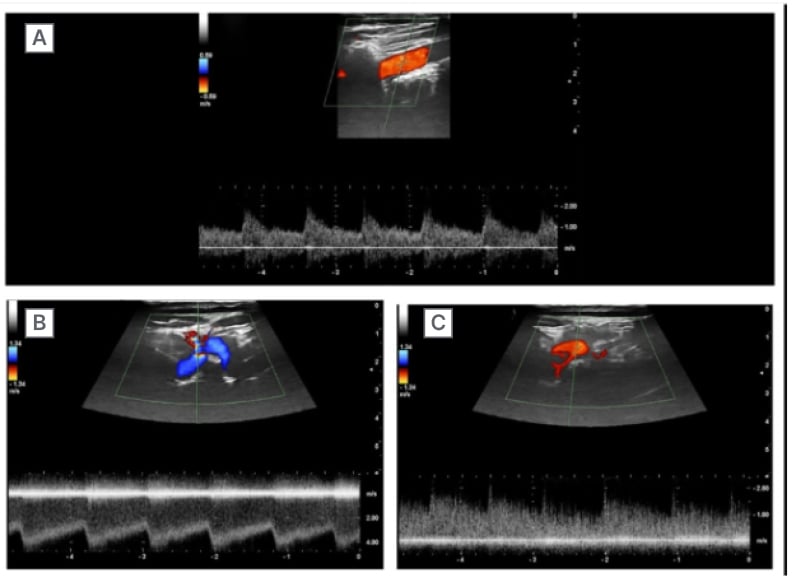
Figure 3: Neurosonological findings in Case 2 (arteriovenous fistula).
A) Extracranial duplex ultrasound of the right VA demonstrating vascular enlargement (7.1 mm diameter), increased PSV and EDV, and reduced resistance index (RI: 0.60).
B) TCCD of the right V3 segment showing abnormal, tortuous arteries with very high flow velocities (PSV: 460 cm/s, EDV: 300 cm/s) and a low pulsatility index (PI: 0.2). Reversed flow from the ipsilateral V4 segment indicates a steal phenomenon.
C) Colour Doppler imaging of arterialised venous drainage into the internal jugular vein and ipsilateral vertebral venous plexus.
EDV: end-diastolic velocity; PI: pulsatility index; PSV: peak systolic velocity; RI: resistance index; TCCD: transcranial colour-coded Doppler; VA: vertebral artery.
Neurosonology was particularly advantageous for establishing the diagnosis of arteriovenous fistula, clarifying the haemodynamic context, and guiding multidisciplinary discussion on the therapeutic approach. The modality provided complementary information to neuroradiological studies, enabling the assessment of dynamic vascular flow patterns not visible on static imaging. The utility of ultrasound in the assessment and management of cerebral arteriovenous malformations, particularly its ability to evaluate real-time haemodynamics and provide insights into shunt flow, has been well-documented in the literature.9,10 The patient is scheduled for endovascular treatment and remains under clinical and neurosonological follow-up.
DISCUSSION
Neurosonology demonstrates remarkable versatility in the assessment of posterior cerebral circulation disorders, as illustrated by the present cases. Its dynamic, real-time evaluation enables not only the identification of stenoses and abnormal flow direction, but also offers insights into collateral circulation, haemodynamic compensation, and the temporal evolution of vascular pathologies. Unlike static radiological modalities, neurosonology allows clinicians to monitor changes over time and observe cerebral haemodynamics in response to physiological or clinical conditions directly at the patient’s bedside. Despite these advantages, certain limitations remain inherent to neurosonological techniques. The reliability of intracranial assessment is still challenged by the absence of universally accepted velocity cut-off values for stenosis grading, particularly within intracranial arteries. The criteria proposed by Baumgartner,11 based on conventional angiography, have long provided a binary classification of stenoses as <50% or >50%. More recently, Danyel et al.8 have advanced the field by introducing thresholds derived from CTA comparison, allowing a clinically relevant distinction between <50%, 50–69%, and severe (70–99%) stenoses, an approach that reflects the risk stratification routinely adopted in stroke care. Furthermore, technical factors such as the inadequacy of the temporal bone acoustic window, especially in elderly and female patients, can limit the feasibility of intracranial insonation. However, evaluation of the VA V4 segment via the suboccipital window generally remains reliable, except in cases with unfavourable neck anatomy.
These considerations underline the importance of integrating neurosonology with neuroradiological imaging. While neurosonology cannot replace advanced radiological techniques, it should be regarded as an essential, complementary diagnostic tool that enriches the overall assessment. The dynamic nature of neurosonology, which provides immediate, repeatable, and physiologically meaningful data, proves invaluable, both for the initial work-up and the longitudinal monitoring of patients with ischaemic and malformative disorders of the posterior cerebral circulation. Thus, neurosonology enables a deeper understanding of the pathophysiology and supports more timely and informed clinical decision-making in real-world practice. It is important to acknowledge that the effectiveness of neurosonology heavily relies on operator skill and comprehensive training, emphasising the need for specialised education and continuous professional development to ensure accurate and reliable assessments.
CONCLUSION
These two cases highlight the remarkable versatility of neurosonology in the investigation of vertebrobasilar disorders with differing pathophysiological backgrounds. By documenting distinctive flow alterations and haemodynamic patterns in vivo, neurosonology proved essential for a nuanced interpretation of posterior circulation pathology. Beyond its established diagnostic value, these observations underscore its role in elucidating complex vascular dynamics and supporting tailored, patient-centred management in both ischaemic and malformative conditions of the vertebrobasilar system. Moreover, due to the operator-dependent nature of neurosonology, ongoing specialised training and continuous education are essential to develop and maintain the skills necessary for optimal diagnostic accuracy.







