BACKGROUND
Immune checkpoint inhibitors (ICI) are used to treat multiple types of cancer. However, there are limited studies on the long-term effects of ICI on fertility. This study seeks to examine factors influencing conception after treatment with ICI and referral rates to the authors’ oncofertility program.1
METHODS
A total of 184 female patients between the ages of 18–45 with malignancies were treated with ICI, from January 2012–December 2023, at a single tertiary medical center. Two patients were excluded due to limited reproductive data. Demographics, oncologic, fertility, and reproductive data were collected and analyzed.
RESULTS
Of the 184 patients, 68 (37.0%) had documented fertility discussions prior to ICI initiation, and 36 (19.6%) patients were referred to reproductive medicine. Of the referred patients, the median age at ICI initiation was 32 years, and 27 (75%) were White. The most common cancers included breast adenocarcinoma (52.8%), hematologic malignancies (25%), and melanoma (13.9%). Twenty-one (58.3%) underwent a fertility preservation cycle (oocyte or embryo cryopreservation). One patient received ovarian stimulation, but oocyte retrieval was not performed due to poor response. There were three patients with successful pregnancies (Table 1). All three were previously treated with nivolumab, and two also received chemotherapy. Of the three patients: one patient used IVF using frozen embryo transfer, to conceive, resulting in two full-term live births; the other two conceived via natural conception, each resulting in one full-term live birth. Time to conception ranged from 12–27 months following ICI completion.
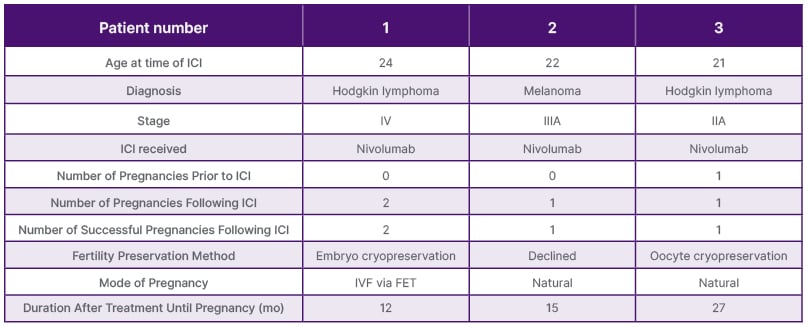
Table 1: Reproductive data for individuals with successful conception following immune checkpoint inhibitors treatment.
FET: frozen embryo transfer; ICI: immune checkpoint inhibitors; mo: months.
CONCLUSION
Early referral to oncofertility providers in young adults with cancer can increase rates of successful conception and increase utilization of fertility preservation methods. Larger, multi-institutional studies are needed to further delineate the long- term effects of ICI on fertility.







