FUSED Deposition Modelling (FDM) 3D printing has become a practical choice for clinical and educational implementation, a 2026 systematic review has found.
It proved a versatile, cost effective, straightforward, and increasingly accessible tool across surgical disciplines, offering an expanding range of medical-grade materials.
3D Printing Processes
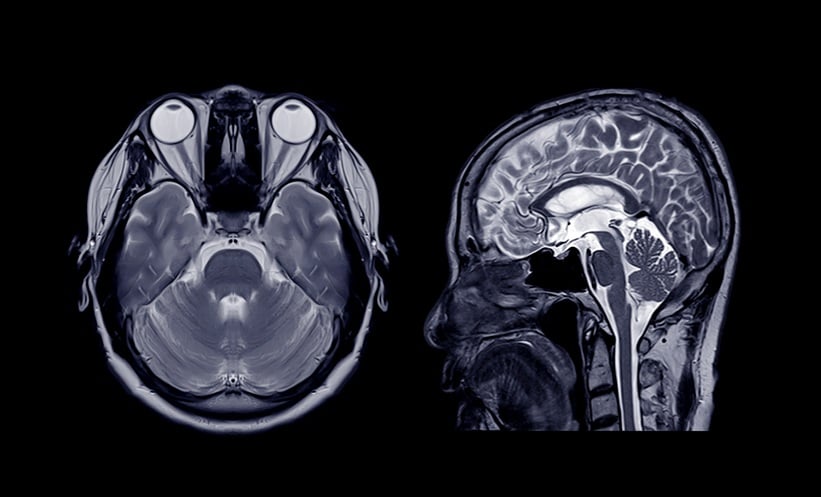
3D printing has gained recent traction in surgical fields and medicine in general. Patient data must first be obtained, usually from CT or MRI scans.
The relevant output from the scan is then converted into stereolitography, a standard computer-aided design format then processed by printer-specific software.
3D Printing in Clinical Settings
The systematic review found that FDM 3D printing technology is increasingly used in routine clinical contexts, exhibiting tangible benefits across surgical planning, training, and device development. Out of an initial near 1,700 records identified, 35 studies met the inclusion criteria.
FDM 3D printing was found to guide and improve preoperative understanding and precision during surgery. For example, models are used in preoperative visualisation, surgical education, and rapid prototyping of patient-specific tools. Studies reported shorter operating times, reduced blood loss, and enhanced procedural confidence, particularly in orthopaedic, spinal, and craniofacial surgery.
Training models created through 3D printing enabled repetitive, risk-free practice at a fraction of the cost of cadaveric or commercial simulators.
It was also found that FDM 3D printing is evolving towards functional, biologically relevant constructs. Thermoplastics are being combined with nanoparticles to enhance biocompatibility and mechanical performance.
FDM 3D printing also proved the most accessible when compared with other methods, especially where sterilisation, material availability, and turnaround time were prioritised.
Practicality Versus Performance
Overall, the systematic review found that FDM 3D printing balances practicality with performance.
While it is characterised by lower resolution and surface detail compared to resin-based methods, clinical differences were found to be minor relative to cost and logistical demands.
The layering process of FDM printing also influenced the durability of guides or prototypes. Researchers suggested that surface roughness might require sanding or solvent smoothing after printing. Very fine features also proved more difficult to consistently reproduce.
Risk of Bias
The heterogeneity of included studies, many of which were feasibility reports, technical notes, or small case series with incomplete reporting, meant direct quantitative comparisons were limited. It follows that the overall evidence base was subject to a high risk of bias.
Clinical Cost-Effectiveness and Reliability
FDM has transitioned from experimental to a widely adopted tool for in-hospital 3D printing. It proves particularly favourable in producing patient-specific anatomical models, cutting guides, and training phantoms.
The field is in rapid development and lacking in established standards, yet the review demonstrates that 3D printing is a reliable and cost-effective tool in preoperative planning, surgical training, device prototyping, and experimental biomaterial development.
Reference
Chrz K et al. Clinical application of FDM 3D printing in surgery and Traumatology: A systematic review. Ann Biomed Eng. 2026;DOI:10.1007/s10439-026-04021-z.