INTRODUCTION
Clinical studies have reported that patients with chronic kidney disease (CKD) with COVID-19 infection have higher hospitalization, ICU admission, and higher mortality compared to patients without CKD. This National Inpatient Sample study aimed to determine the impact of CKD on the severity of outcomes with COVID-19 infection.1-3
METHODS
The authors identified patients hospitalized with COVID-19 infection and a history of CKD from the 2020–2021 National Inpatient Sample database. STATA/MP 17.0 software (StataCorp LLC., Texas, USA)was used for statistical analysis. Multivariate logistic regression analysis was then performed.
RESULTS
There was a total of 818,011 patients hospitalized with COVID-19 infection and 407,312 patients with a history of CKD (Tables 1 and 2). The patients with COVID-19 infection were stratified based on their CKD status. Among them, 787,351 patients had COVID-19 infection without CKD, while 30,660 patients had both COVID-19 infection and CKD. The mean age was 61.2 years for patients with COVID-19 infection without CKD, compared to 73.2 years for those with CKD. People who are White constituted the largest ethnic group in both categories. Patients, in the lowest income quartile and those with Medicaid insurance, constituted the largest group among patients constituted the largest group among the national income quartile and insurance groups, respectively, in both categories. The length of hospital stay was 9.3 days for patients with COVID-19 infection without CKD and 8.2 days for those with CKD (p<0.001). The mortality rate was 12.7% among patients with COVID-19 infection without CKD and 22.5% for those with CKD (p<0.001). The unadjusted odds ratio (OR) of mortality in patients with COVID-19 infection with CKD was 1.99. After adjustment for age, sex, race, Charlson comorbid index, national income quartile, and insurance, the adjusted OR of mortality was 1.03 (p<0.001), indicating that the mortality rate was significantly higher among patients with COVID-19 infection with CKD, compared to those without CKD. The unadjusted OR for invasive ventilation in patients with COVID-19 infection with bronchiectasis was 1.26, and the adjusted OR was 0.89 (p<0.001), indicating that the need for invasive ventilation was significantly lower in patients with CKD.
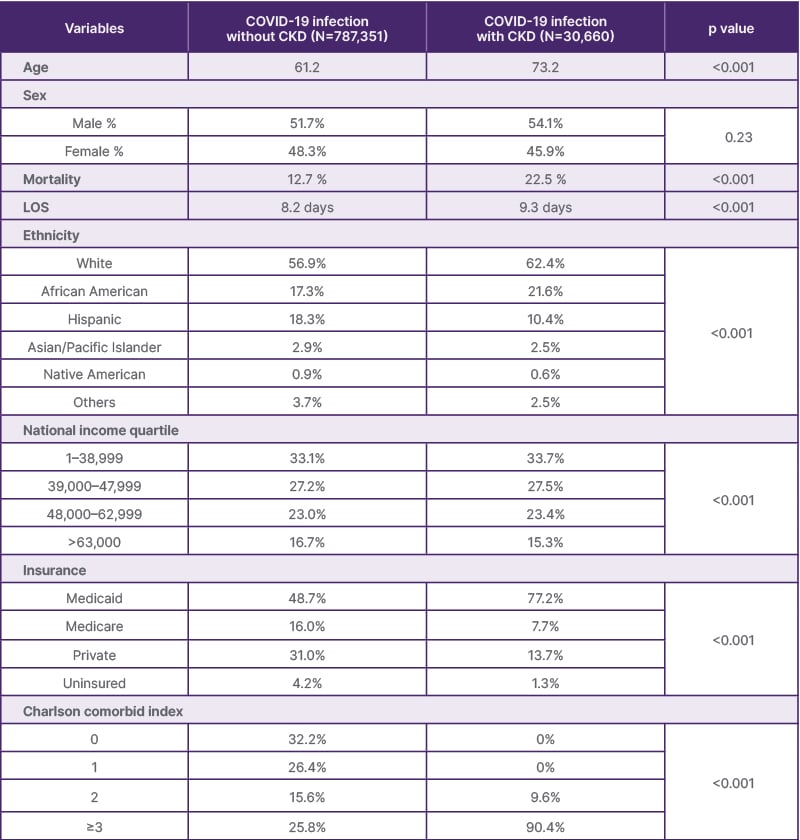
Table 1: Demographic and clinical characteristics from the 2020-2021 National Inpatient Sample database.
LOS: length of stay.
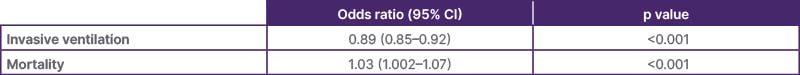
Table 2: Outcomes and adjusted odds ratio.
CONCLUSION
The authors’ analysis of the National Inpatient Sample database suggests that CKD was a significant risk factor for severe COVID-19 infection. Patients with both COVID-19 infection and CKD had longer lengths of stay, a lower need for invasive ventilation, and a higher mortality rate compared to those without CKD.







