BACKGROUND
The Surviving Sepsis Campaign Guidelines recommend the use of inotropic agents, such as dobutamine, for patients with septic shock and cardiac dysfunction. However, previous studies have demonstrated that a considerable proportion of these patients do not tolerate dobutamine well. Identifying predictors that indicate a favorable response to dobutamine remains an important yet unclear area of investigation.
METHODS
This single-center, retrospective cohort study (2011–2020) examined adult patients admitted to a quaternary ICU with septic shock, who were started on dobutamine within 72 hours of receiving an echocardiogram.1 Baseline characteristics, echocardiographic data, and serial norepinephrine equivalent (NEE) doses were collected at dobutamine initiation, as well as at 2 and 6 hours post-initiation.
RESULTS
Eighty-two patients met the inclusion criteria, of whom 48% were female. The median age was 66 years (interquartile range [IQR]: 54–75), and the median Acute Physiology, Age, Chronic Health Evaluation (APACHE) III score was 115 (IQR: 97–140). The median lactate level was 5.6 (IQR: 3.1–9.4), with a median fluid balance of 3,634 mL (IQR: 1,645–6,290). The median left ventricular ejection fraction (LVEF) was 35% (IQR: 25–55), and the median left ventricular outflow tract (LVOT) velocity-time integral (VTI) was 12.1 cm (IQR: 9.3–15.0). Of all the patients, 73% were initiated on 2.5 mcg/min of dobutamine, with a median NEE at dobutamine initiation of 0.24 mcg/kg/min (IQR: 0.15–0.62). In-hospital mortality in all patients was 58.5%. Univariate analysis suggested in-hospital mortality to be higher in patients with a higher admission APACHE III score (101 [IQR: 87–119] versus 131[105, 143]; p<0.001) and a lower LVOT VTI (13.3 [IQR: 10.8–17.5] versus 11.3 [IQR: 8.4–13.9]; p=0.05). LVEF, cardiac output, systematic vascular resistance, and heart rate were not associated with in-hospital mortality. Based on the LVOT VTI groups (LVOT VTI <12 cm versus LVOT VTI ≥12 cm), an assessment of NEE dosage upon dobutamine initiation indicated a trend towards a better response in patients with LVOT VTI <12 cm (Figure 1A). Multivariable-adjusted logistic regression suggested that a lower LVOT VTI at dobutamine initiation was associated with improved outcomes (Figure 1B).
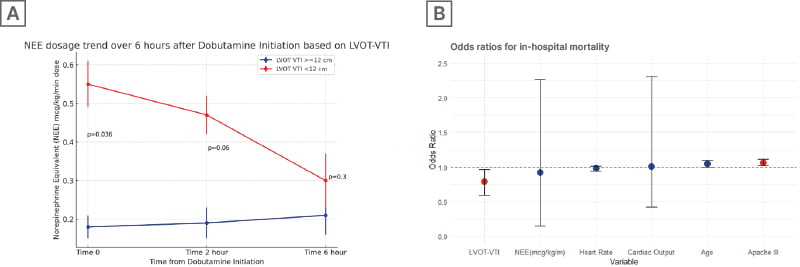
Figure 1: Norepinephrine equivalent dosage trend (A) and in-hospital mortality (B).
A) Norepinephrine equivalent dosage trend over 6 hours after dobutamine initiation based on left ventricular outflow tract velocity-time integral; B) Odds ratios for in-hospital mortality.
LVOT-VTI: left ventricular outflow tract velocity-time integral; NEE: norepinephrine equivalent.
CONCLUSION
Although guidelines support dobutamine in septic shock with cardiac dysfunction, there is limited guidance on optimal predictors for their use. The authors’ findings suggest a potential trend for reduced NEE requirements and in-hospital mortality when dobutamine is used in patients with LVOT VTI <12 cm. Larger studies are needed to validate these results and inform indications for inotropic therapy.







