INTRODUCTION
Atrial fibrillation/flutter (AF) is a common early post-operative complication after lung transplantation (LTX) and has been associated with increased morbidity and mortality. Optimal management has not been established. Some studies have suggested increased mortality with the use of amiodarone. The authors’ standard approach is early rhythm control with amiodarone followed by cardioversion if needed. Anticoagulation is withheld if sinus rhythm is restored within 48 hours.
The authors sought to review their experience to determine if the occurrence of AF was associated with increased morbidity and/or mortality, and specifically, if survival was lower with the use of amiodarone.
METHODS
Adult LTX recipients with AF occurring during the index transplant hospital stay were identified. Characteristics of these patients were compared with a contemporaneous cohort without AF. Wilcoxon rank-sum tests were used to compare length of stay (LOS), duration of mechanical ventilation, and age at time of transplant. Fisher’s exact tests were used to evaluate acute kidney injury and primary graft dysfunction. Post transplant survival was compared with log-rank analysis of Kaplan-Meir estimates.
RESULTS
Between September 2017 and October 2024, 104 out of 294 (35%) LTX recipients developed post-operative AF. The AF group was slightly older (67.7 years versus 64.9 years; p=0.0002), but otherwise similar to the non-AF cohort with respect to gender, comorbidities, underlying disease, and transplant type. Both ICU LOS (median 6.5 days versus 3.5 days; p<0.001), and total hospital LOS (21 days versus 16 days; p<0.001) were longer in the AF group. The AF group had a higher incidence of acute kidney injury of any severity (46% versus 27%; p=0.002) and any grade of primary graft dysfunction (53% versus 42%; p=0.12). Eighty (77%) patients with AF received amiodarone therapy, 16 (15%) underwent cardioversion, and 15 (14%) were anticoagulated. Survival at 1, 3, and 5 years post-transplant was 94%, 86%, and 79%, respectively, in the AF group, compared to 97%, 93%, and 80% in the non-AF cohort (p=0.36). Among subjects treated with amiodarone, survival was 92%, 83%, and 74% at 1, 3, and 5 years, respectively (p=0.19 versus no AF; Figure 1).
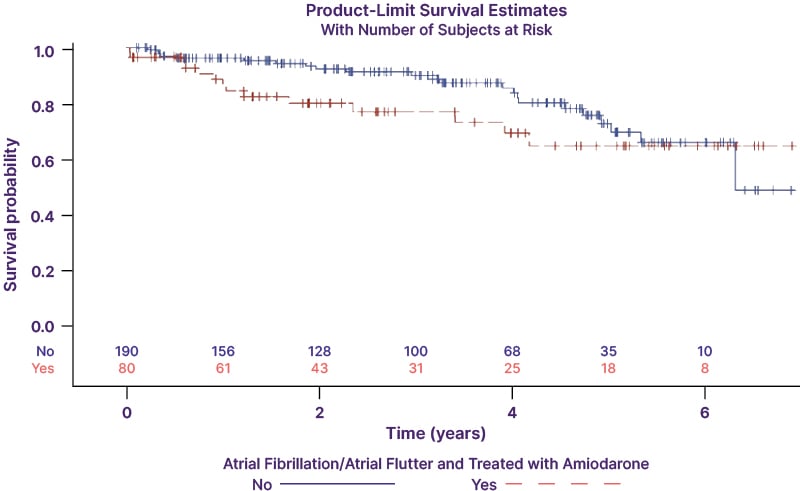
Figure 1: Survival of patients with atrial fibrillation/atrial flutter treated with amiodarone, compared to patients with no atrial fibrillation/atrial flutter.
CONCLUSION
Early post-transplant AF is associated with longer LOS and higher incidence of acute kidney injury; however, long-term survival was comparable to recipients without AF. Amiodarone use was not associated with increased mortality. Additional studies are required to determine the optimal approach to the prevention and management of post-operative AF after LTX.







