BACKGROUND AND OBJECTIVES
Patients with COPD who survive sepsis remain immunocompromised and are at increased risk of subsequent viral infections, including influenza and respiratory syncytial virus (RSV).1-3 However, the risk of viral infections among patients with COPD after sepsis remains unclear.4-5 This real-world data study aimed to investigate the 1-year risk of viral infections among patients with COPD, following sepsis.
MATERIALS AND METHODS
The authors used the TriNetX (Cambridge, Massachusetts, USA) platform, which integrates anonymized clinical data from 92 healthcare organizations, to identify 113,589 patients with COPD and sepsis. The risk of distinct viral infections, including herpes simplex virus (HSV), varicella-zoster virus (VZV), cytomegalovirus (CMV), RSV, and influenza, within 1-year post-sepsis was analyzed, with 1:1 propensity score matching employed to minimize confounding. The effect of vaccination was also assessed to determine their protective efficacy.
RESULTS
A total of 98,883 patients with COPD and sepsis and 1:1 matched patients with COPD without sepsis were eligible for analyses. Table 1 shows that patients with COPD and sepsis had a consistently higher risk of distinct viral infections within 1-year post-sepsis. Specifically, HSV occurred in 1.36% of the sepsis cohort versus 0.83% of controls (hazard ratio [HR]: 1.936; 95% CI: 1.775–2.112); VZV in 0.34% versus 0.13% (HR: 3.050; 95% CI: 2.489–3.737); CMV in 0.58% versus 0.32% (HR: 2.101; 95% CI: 1.832–2.410); RSV in 7.67% versus 2.86% (HR: 3.297; 95% CI: 3.158–3.443); and influenza in 8.62% versus 3.34% (HR: 3.197; 95% CI: 3.071–3.328). Among the five viral infections, RSV and influenza exhibited the highest absolute and relative risks, representing the greatest viral burden in the post-sepsis setting. Sensitivity analyses revealed that the increased post-sepsis risks for viral infections remained consistent across various sepsis severities, including cases involving bacteremia, vasopressor use, mechanical ventilation, or hemodialysis. Additionally, the authors examined the protective effects of vaccinations in patients with COPD, and found significant risk reduction associated with the VZV glycoprotein E vaccine (HR: 0.724; 95% CI: 0.595–0.882), the RSV prefusion F protein-based vaccine (HR: 0.676; 95% CI: 0.563–0.812), and the influenza vaccine (HR: 0.709; 95% CI: 0.649–0.776).
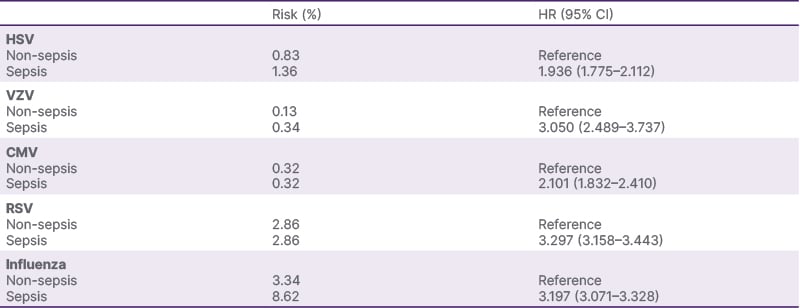
Table 1: One-year risk of distinct viral infections between 98,883 patients with COPD and sepsis, and propensity score-matched patients with COPD without sepsis.
CMV: cytomegalovirus; HR: hazard ratio; HSV: herpes simplex virus; RSV: respiratory syncytial virus; VZV: varicella zoster virus.
CONCLUSION
In this study, the authors used a federated database to identify the increased one-year risk of viral infections, including HSV, VZV, CMV, RSV, and influenza, following sepsis in patients with COPD. Furthermore, the authors demonstrated the protective effect of vaccination against influenza and RSV. The findings underscore the need for heightened vigilance regarding viral infections in patients with COPD who have survived sepsis and support the prioritization of vaccination in COPD management strategies, particularly among patients with stable disease. Further prospective studies are warranted to validate these findings and to elucidate the post-septic immunological alterations in patients with COPD.







