Meeting Summary
Bronchiectasis is a progressive respiratory condition that contributes to significant morbidity, reduced quality of life, and increased healthcare utilisation. At the European Respiratory Society (ERS) Congress held in Amsterdam, the Netherlands, from 27th September–1st October 2025, three posters were presented offering real-world, routine-care insights into the clinical characteristics, treatment patterns, and exacerbations of patients with bronchiectasis across the UK, France, and Japan. Michael R. Loebinger, Professor of Practice (Respiratory Medicine) at Imperial College London, and Consultant Respiratory Physician at Royal Brompton Hospital, London, UK; Pierre-Régis Burgel, Professor of Respiratory Medicine at the Hôpital Cochin AP-HP and Université Paris Cité, France; and Takanori Asakura, Assistant Professor in the Division of Pulmonary Medicine at Keio University School of Medicine, Tokyo, Japan, presented recent real-world data from the UK, France, and Japan, respectively.
Overall Summary
The findings of three retrospective studies provide valuable insights into the burden of bronchiectasis across different healthcare settings geographically.1-3 In the UK and France, patients who experienced ≥2 exacerbations during baseline were more likely than those with <2 exacerbations to present with comorbidities, including asthma in the UK and COPD in both countries, and to carry a greater treatment burden.1,2 Moreover, the presence of ≥2 exacerbations, COPD, or asthma in the UK and having ≥2 exacerbations or COPD in France during baseline was associated with an increased risk of further exacerbations during follow-up.1,2 Significant burden of exacerbations was also presented in Japan, regardless of age or preexisting respiratory diseases.3 Taken together, these studies highlight the unmet need for effective management strategies aimed at reducing and preventing exacerbations as a means of alleviating the overall burden of bronchiectasis.1-3
Background
Bronchiectasis is a chronic, progressive, and inflammatory respiratory condition characterised by permanent dilatation of the bronchi, and is typically associated with persistent cough, sputum production, and exacerbations.4 Pulmonary exacerbations experienced by patients with bronchiectasis necessitate antibiotic therapy or hospitalisation, thereby contributing to the substantial disease burden and high utilisation of healthcare resources.4,5 Updated ERS guidelines define patients at high risk of exacerbations as those having a history of ≥2 exacerbations in the prior year or one severe exacerbation or one exacerbation plus severe daily symptoms.6
Existing evidence in the USA and Europe has demonstrated that exacerbations are associated with considerable morbidity, including heightened hospitalisation rates and impaired quality of life.7,8 Despite these insights, there remains a paucity of research examining morbidity and treatment patterns explicitly related to bronchiectasis exacerbations in the UK, France, and Japan.
Morbidity in Patients with Non-cystic Fibrosis Bronchiectasis and Exacerbations in The Health Improvement Network® (Cegedim, Paris, France) UK and France Databases1,2
Two studies explored the association of exacerbations with morbidity and treatment patterns among patients with bronchiectasis in the UK and France, respectively, using primary care electronic health record (EHR) data.
Methodology
Two retrospective studies using data from 2018 to the end of 2022 were conducted via The Health Improvement Network (THIN) UK and France, respectively; comprehensive longitudinal databases comprising EHR extracts recorded by primary care physicians. Eligible participants were individuals aged 12 years or older who had a diagnosis of bronchiectasis in 2018 without cystic fibrosis.
Study assessments included patient demographics, comorbidities, and treatment patterns. Exacerbations were defined as primary care physician visits with codes for exacerbations, haemoptysis, lower respiratory tract infection, or antibiotic prescription with either bronchiectasis or ≥1 lower respiratory tract infection symptom. Exacerbation incidence during follow-up was estimated using the Kaplan–Meier method, while the association of baseline characteristics with exacerbations at follow-up was estimated using hazard ratios by means of a multivariable Cox model.
Clinical Characteristics
A total of 12,106 patients were included in the UK and 6,194 in France, of which 1,881 (15.5%) and 774 (12.5%), respectively, experienced ≥2 exacerbations during baseline (Table 1). Patients with ≥2 exacerbations during the baseline period were significantly more likely to have comorbidities such as asthma, COPD, gastro-oesophageal reflux disease, and heart failure compared with those with <2 exacerbations (Table 1).
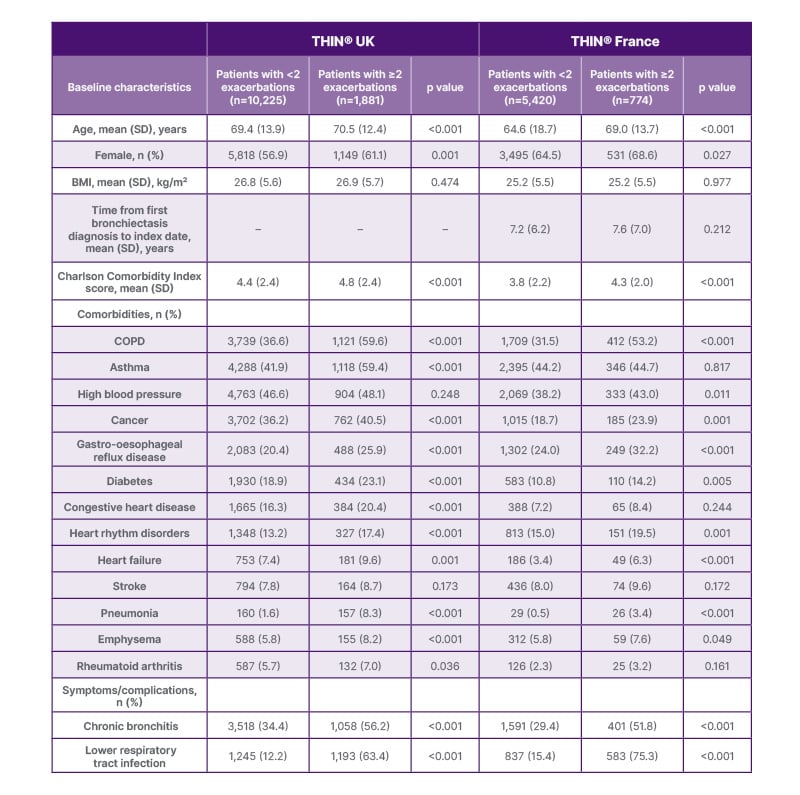
Table 1: Demographics and comorbidities during the 12-month baseline period (2018).
THIN®: The Health Improvement Network® (Cegedim, Paris, France).
Exacerbation Risk Factors
Approximately 70% of patients in the UK and 75% of patients in France with ≥2 exacerbations during the baseline period experienced a subsequent exacerbation within the first year of follow-up. This compares with only around 30% and 25% of patients in the UK and France, respectively, who had <2 exacerbations during baseline (Figure 1).
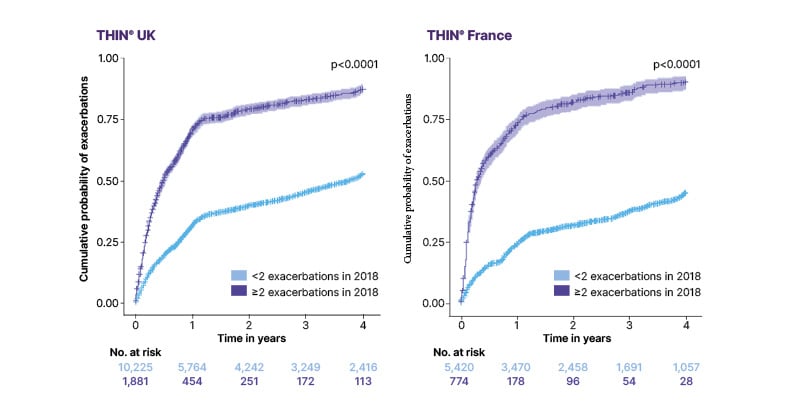
Figure 1: Risk of exacerbations during follow-up by exacerbation frequency during the baseline period (2018).
No: number; THIN®: The Health Improvement Network®.
After adjusting for covariates, the presence of ≥2 exacerbations during baseline was associated with a 160% increased risk of further exacerbations during follow-up in the UK and a 309% increased risk in France (Table 2). In the UK, the presence of COPD was also associated with a 48% increased risk of further exacerbations, while asthma increased the risk by 21%. In France, COPD and heart failure at baseline increased the risk of further exacerbations by 27% and 21%, respectively.
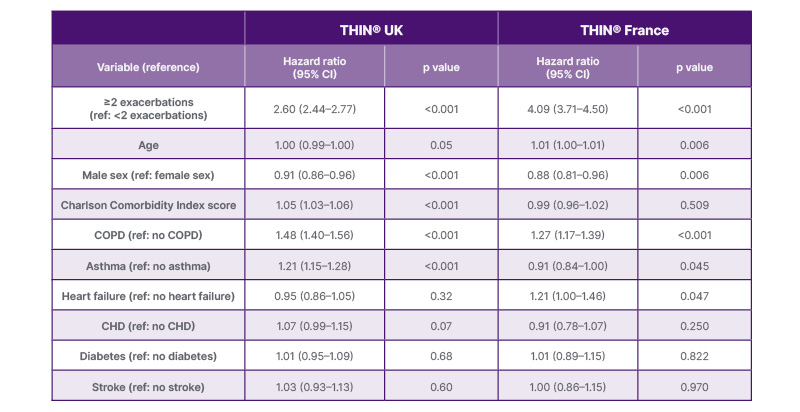
Table 2: Risk of exacerbations during follow-up by characteristics and comorbidities during the baseline period (2018).
CHD: congestive heart disease; ref: reference; THIN®: The Health Improvement Network®.
Treatment Patterns
In both the UK and France, patients who experienced ≥2 exacerbations during baseline were more likely to have received treatments such as antibiotics (oral and inhaled), inhaled corticosteroids, oral steroids, mucolytics, and bronchodilators, either at baseline or during follow-up, compared with those with <2 exacerbations. The use of long-term antibiotics remained consistent between 2018–2022 among patients with ≥2 exacerbations during baseline in the UK, with approximately one in four patients receiving these therapies (23.8% and 24.5%, respectively). In France, although the overall antibiotic prescriptions declined over time in patients with ≥2 exacerbations, from 91.9% of patients in 2018 to 80.4% in 2022, the use of long-term antibiotics remained relatively stable across this period (15.5% versus 13.5%, respectively).
Limitations
Several limitations should be considered when interpreting these findings. First, a database-specific definition of exacerbations was employed to minimise the likelihood of false-positive classifications. As a result, the actual exacerbation frequency in clinical practice may be higher, particularly as self-managed episodes were unlikely to be captured in EHRs. Second, data were derived exclusively from participating primary care sites with no linkage to secondary care hospital data; thus, exacerbations or treatments managed in hospital settings may not have been represented. Finally, treatment patterns observed during follow-up may have been influenced by the COVID-19 pandemic, which disrupted healthcare utilisation globally, as well as the loss of some patients at follow-up.
Conclusion
Data from the THIN UK and France databases reveal that patients with bronchiectasis who had ≥2 exacerbations during the baseline period were at the highest risk of experiencing exacerbations during follow-up. In addition, patients with ≥2 exacerbations during baseline had more comorbidities, including asthma in the UK and COPD in both countries, and a higher overall treatment burden than those with <2 exacerbations. Overall, these data illustrate the importance of effective strategies aimed at reducing and managing exacerbations as a means of alleviating the overall burden of bronchiectasis.
Exacerbations Among Incident Cases of Bronchiectasis in Japan3
This study was conducted to evaluate bronchiectasis-associated exacerbations over incident cases and in subgroups of patients with preexisting respiratory diseases in Japan.
Methodology
This retrospective analysis utilised two administrative claims databases provided by JMDC, Inc., Tokyo, Japan, which included insured individuals aged <75 years from February 2015–April 2023 and aged ≥75 years from April 2019–March 2023.
Patients with bronchiectasis were identified according to claims-based diagnostic criteria. Incident cases with bronchiectasis, defined as meeting bronchiectasis diagnosis criteria (index date) and without any other bronchiectasis-related claim in the year prior to the index date, were included.
Study outcomes of interest were pulmonary exacerbations, defined as either a bronchiectasis-related hospitalisation or bronchiectasis-related ambulatory visit followed by administration of oral or intravenous (IV) antibiotics. Exacerbations were further categorised into those requiring oral antibiotic use and those requiring hospitalisation or IV antibiotic therapy. The burden of bronchiectasis during follow-up was quantified by examining the proportion of patients who experienced exacerbations, the annualised rate of exacerbations, and the time from index +1 day to first exacerbation.
Results
A total of 6,288 patients aged <75 years and 1,127 patients aged ≥75 years identified as incident cases of bronchiectasis were included in the analysis. Compared with those aged <75 years, a higher proportion of patients aged ≥75 years had all-cause hospitalisations, respiratory-related hospitalisations, and long-term macrolide use during the 1-year period prior to the diagnosis of non-cystic fibrosis bronchiectasis.
Exacerbation outcomes during the follow-up period are summarised in Table 3. Overall, 63.6% of patients aged <75 years (mean follow-up duration of 2.8 years) and 67.2% of patients aged ≥75 years (mean follow-up of 1.4 years) experienced at least one exacerbation. The proportion of patients who required hospitalisation or IV antibiotics for an exacerbation was approximately three times higher in the ≥75-year group compared with the <75-year group (67.6% versus 23.0%, respectively). Similarly, the annualised rate of exacerbations requiring hospitalisation or IV antibiotics was around six times higher among patients aged ≥75 years than among those aged <75 years (0.43 versus 0.07 per person-year, respectively).
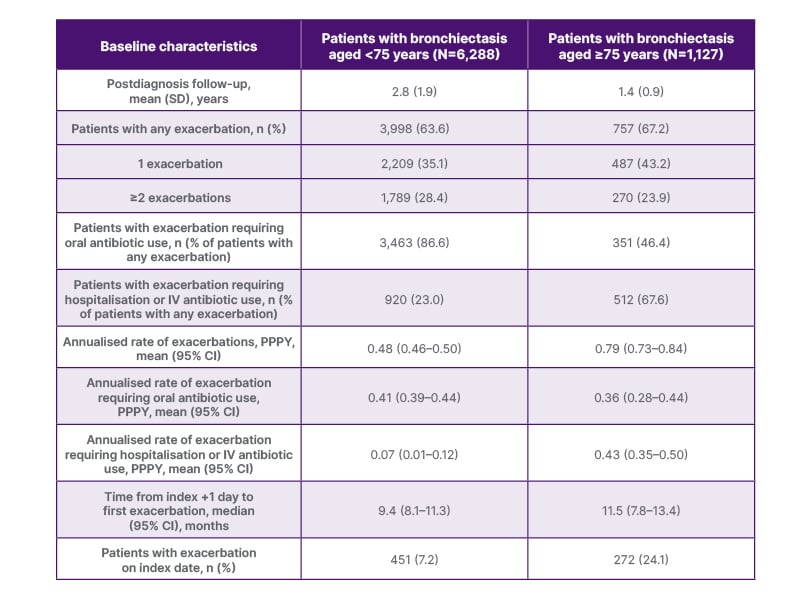
Table 3: Pulmonary exacerbations among incident cases of bronchiectasis in Japan.*
*Baseline risk factors associated with ≥2 exacerbations during follow-up were assessed using multivariate regression analysis. The risk factors were bronchitis, GORD, COPD, asthma treated with ICS, pneumonia, chronic rhinosinusitis, long-term macrolide use, NTM-PD, and idiopathic lung disease in patients aged <75 years; and pneumonia, long-term macrolide use, and idiopathic interstitial lung disease in patients aged ≥75 years (with an OR with a p value <0.05).
GORD: gastro-oesophageal reflux disease; ICS: inhaled corticosteroids; IV: intravenous; NTM-PD: nontuberculous mycobacterial pulmonary disease; OR: odds ratio; PPPY: per person per year.
Compared with the full population, the patients with pre-existing respiratory diseases (COPD, asthma, nontuberculous mycobacterial pulmonary disease, or chronic rhinosinusitis) presented higher proportions of patients with exacerbations, higher annualised rates, and a shorter time to first exacerbation, leading to a greater burden of exacerbations. Trends in exacerbations were generally similar across both age cohorts in the four subpopulations.
Limitations
There are several limitations of this study that should be considered. First, underreporting of pulmonary exacerbations may result from the absence of claims with bronchiectasis International Classification of Diseases (ICD) codes. Second, the incident cases were required to have only a 1-year washout period without any claims with a bronchiectasis diagnosis, which may have resulted in the inclusion of prevalent cases with earlier diagnoses. Conversely, patients with a relatively shorter disease history may have experienced fewer exacerbations, leading to potential underestimation of the overall exacerbation burden. Finally, the study period encompassed the COVID-19 pandemic, during which declines in non-COVID-19 respiratory-related hospitalisations were reported. This phenomenon may have contributed to the underreporting of bronchiectasis-related hospitalisations.
Conclusion
This first large-scale, real-world, population-based study analysed exacerbations among incident patients with bronchiectasis across all age populations in Japan. The findings demonstrate a substantial burden of exacerbations, evident irrespective of patient age or the presence of preexisting respiratory diseases. These results underscore the unmet need for effective management strategies aimed at reducing or preventing exacerbations in order to lessen the overall burden of bronchiectasis in Japan.
MED-ALL-BE-00048 October 2025







