BACKGROUND AND AIMS
Most studies on juvenile idiopathic arthritis (JIA) aetiology are case-control studies, which are susceptible to recall and selection bias. A meta-analysis of 66 environmental factors (including 11 cohort and 28 case-control studies), concluded that a caesarean section (C-section) increases JIA risk, while the presence of siblings lowers it.1
The aim of the authors was to examine birth-related factors in relation to JIA risk using two large prospective cohorts to provide more robust evidence.2
METHODS
The authors used data from two population-based cohorts linked to various health registries: 1) the MoBa study, a pregnancy cohort with data from >114,000 mother–child pairs;3 and 2) the Norwegian National Registry Linkage Cohort (NRC), a cohort based on all births in Norway from 2004–2020, with complete data from the Norwegian Medical Birth Registry.
A JIA case was defined as ≥2 International Classification of Diseases, 10ᵗʰ Revision (ICD-10) codes (≥2 M08, ≥2 M09, or 1 M08 and 1 M09) by linking both cohorts to the Norwegian Patient Registry. Exposure variables included parity, mode of delivery, birth weight (in 500 g increments), delivery timing, and season of birth. The authors used multivariable logistic regression analyses, which were reported as adjusted odd ratios (aOR) with 95% CIs. Potential confounders are listed in the legend of Table 1. The authors also stratified their analyses by sex to observe any sex differences.
RESULTS
In the MoBa study, the final analytical sample included 279 mothers of children who later developed JIA, and 85,887 mothers of children who did not. The NRC included 969 mothers of children who later developed JIA, and 779,231 mothers of children who did not. No robust associations were found between parity or birth weight and JIA. Elective C-section versus vaginal birth was positively associated with JIA in the MoBa study (aOR: 1.58; 95% CI: 1.02–2.45), but not in the NRC. Regarding the MoBa study, the authors found a negative association between post-term delivery and JIA (aOR: 0.55; 95% CI: 0.31–0.98), whereas in the NRC, there was a negative association between preterm delivery and JIA in girls (aOR: 0.67; 95% CI: 0.45–1.00). Autumn versus winter births were positively associated with JIA in girls in the MoBa study (aOR: 1.54; 95% CI: 1.01–2.34), with no other seasonal effects observed (Table 1).
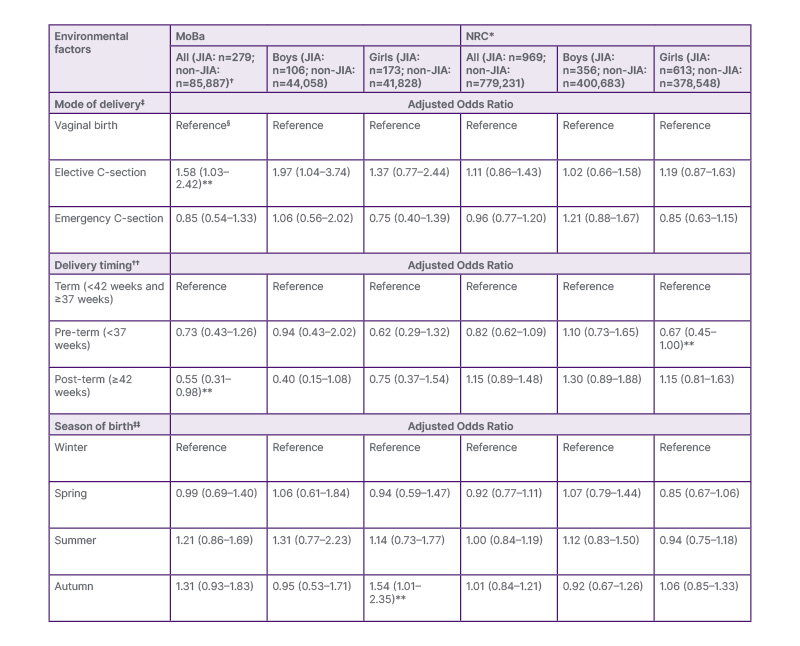
Table 1. Associations between birth-related factors and juvenile idiopathic arthritis in the National Registry Linkage Cohort (or Million Baby Cohort) and MoBa.
*The authors lacked data on the maternal history of rheumatic disease in NRC, and did not adjust for it in those analyses.
†One non-JIA case is missing from the data presented in the table, as the sex of this individual was not specified, and therefore was not included during sex stratification.
‡Adjusted for maternal education, history of rheumatic disease, region of birth, birth year, gestational smoking, maternal age, parity, and birth weight.
§Mentions of ‘reference’ in the table indicate a point of comparison when presenting the data.
**Statistically significant results.
††Adjusted for all in one plus mode of delivery, except history of rheumatic disease and birth weight.
‡‡Adjusted for maternal education only.
C-section: caesarean section; JIA: juvenile idiopathic arthritis; NRC: National Registry Linkage Cohort.
CONCLUSION
To the best of the authors’ knowledge, their study is the largest prospective study exploring how birth-related environmental factors are associated with the risk of JIA. They found an increased risk with elective, but not acute, C-section in one cohort, which was consistent with prior findings,1,4 but did not reach significance in the other cohort. This suggests a potential role for intestinal microbiota in JIA development. The authors also observed trends towards negative associations with pre- and post-term births and JIA, warranting further investigation. A positive association between autumn births and JIA risk in girls was observed in one cohort, highlighting the potential sex-specific effects of seasonal factors. The difference in results between the two cohorts may reflect time trends.







