BACKGROUND AND AIMS
This study aimed to perform a multifactorial comparison of the surgical outcomes of mini-percutaneous nephrolithotomy (mini-PNL) and flexible ureterorenoscopy (fURS) in the treatment of patients with solitary renal pelvic stones measuring 1–2 cm and having a stone density of >1,000 Hounsfield units.1
MATERIALS AND METHODS
The authors retrospectively analysed 79 patients who underwent either mini-PNL (n=23) or fURS (n=56) between January 2018–December 2023 at the Department of Urology, SBÜ Adana City Training and Research Hospital, Türkiye.
All patients had a solitary renal pelvic stone measuring 1–2 cm with a density exceeding 1,000 Hounsfield units, confirmed by pre-operative, non-contrast CT. Routine pre-operative preparations, including urine culture, laboratory tests, chest X-ray, and ECG, were performed.
The following parameters were evaluated:
- demographics: age, gender, BMI, and American Society of Anesthesiologists (ASA) score;
- stone characteristics: laterality, size (length, area, and volume), opacity, and density;
- operative factors: fluoroscopy time, operative time, and hospital stay;
- laboratory parameters: pre-operative and postoperative Day 1 serum creatinine, estimated glomerular filtration rate, haematocrit, and white blood cell counts; and
- clinical outcomes: stone-free rates, postoperative Day 1 and 1-month residual stone rates, post-operative Visual Analogue Scale (VAS) scores (1st, 6th, 12th, and 24th hour), and complications classified according to the Clavien-Dindo grading system.
RESULTS
Among the 79 patients, 23 underwent mini-PNL and 56 underwent fURS (Table 1). In terms of gender distribution, there were seven females and 16 males in the mini-PNL group compared to 24 females and 32 males in the fURS group (p=0.304). The mean age was 51.0±15.8 years in the mini-PNL group compared to 48.1±14.8 years in the fURS group (p=0.44). The mean BMI was significantly higher in the fURS group (27.5±4.8 kg/m2) compared to the mini-PNL group (25.8±2.5 kg/m2; p=0.04). In terms of stone characteristics, stone size, area, and volume were significantly larger in the mini-PNL group (p<0.05). Fluoroscopy time was significantly longer in the mini-PNL group (75.2±55.2 seconds) compared to the fURS group (12.7±7.9 seconds; p<0.001). The operative time was also significantly longer in the mini-PNL group (97.8±27.9 minutes) compared to fURS (65.7±23.8 minutes; p<0.001). Hospital stay was significantly shorter in the fURS group (1 day) compared to the mini-PNL group (3 days; p<0.001). Post-operative VAS scores were significantly lower in the fURS group at all time points (p<0.001). Post-operative haematocrit decrease was more pronounced in the mini-PNL group (p=0.033). Stone-free rates were comparable between groups; residual stones were found in 17.4% of mini-PNL cases compared to 8.9% of fURS cases (p=0.282). No significant differences were observed in post-operative creatinine, estimated glomerular filtration rate, or white blood cell levels.
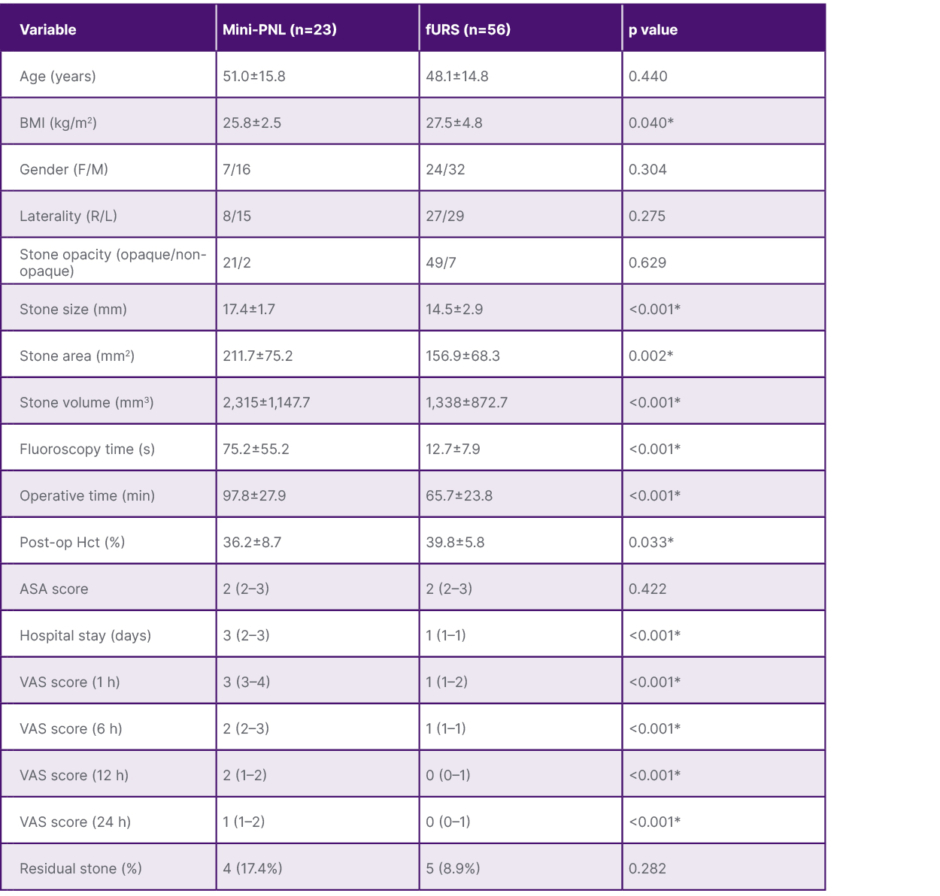
Table 1: Comparative analysis of 1–2 cm hard pelvic stones.
*p<0.05 is statistically significant.
ASA: American Society of Anesthesiologists; F: female; fURS: flexible ureterorenoscopy; Hct: haematocrit; L: left; M: male; Mini-PNL: mini-percutaneous nephrolithotomy; post-op: post-operative; R: right; VAS: Visual Analogue Scale.
CONCLUSION
For the management of hard and solitary renal pelvic stones measuring 1–2 cm, both mini-PNL and fURS achieve comparable stone-free rates. However, fURS offers significant advantages in terms of shorter operative time, less fluoroscopy exposure, reduced post-operative pain, and a shorter hospital stay, making it a safer and less invasive alternative in appropriately selected cases.







