BACKGROUND AND AIMS
Radical prostatectomy in patients with a history of transurethral resection of the prostate (TUR-P) can be technically challenging due to altered surgical anatomy. This study aimed to present the outcomes of robot-assisted laparoscopic radical prostatectomy (RARP) in patients with prior TUR-P.1
METHODS
A retrospective review was conducted of 11 patients with a history of TUR-P who were diagnosed with prostate cancer via TRU-CUT biopsy due to elevated prostate-specific antigen levels, and who underwent RARP between 2018–2024. Demographic, perioperative, pathological, oncological, and functional data were analysed. Continence was defined as using less than one pad per day, and erectile function was evaluated using the International Index of Erectile Function-5 (IIEF-5) scores.
RESULTS
The mean age was 63.54 years, with a mean pre-operative prostate-specific antigen of 7.17 ng/mL and a mean prostate volume of 142 cc (Table 1). The mean console time was 149 minutes, the mean blood loss was 29 mL, and the mean hospital stay was 5.3 days. No positive surgical margins were observed. Gleason scores were 3+3 in 73% of patients, 3+4 in 9%, and 4+3 in 18%. Perineural invasion was present in 54% of patients, seminal vesicle invasion in 9%, and extraprostatic extension in 9%. Mean follow-up was 50.7 months, during which biochemical recurrence occurred in one patient (9%) at Month 40. At 1-year follow-up, all patients achieved continence. A pre-operative IIEF-5 score >22 was present in 27% of patients, which decreased to 9% post-operatively and improved to 36% after intracavernosal injection therapy.
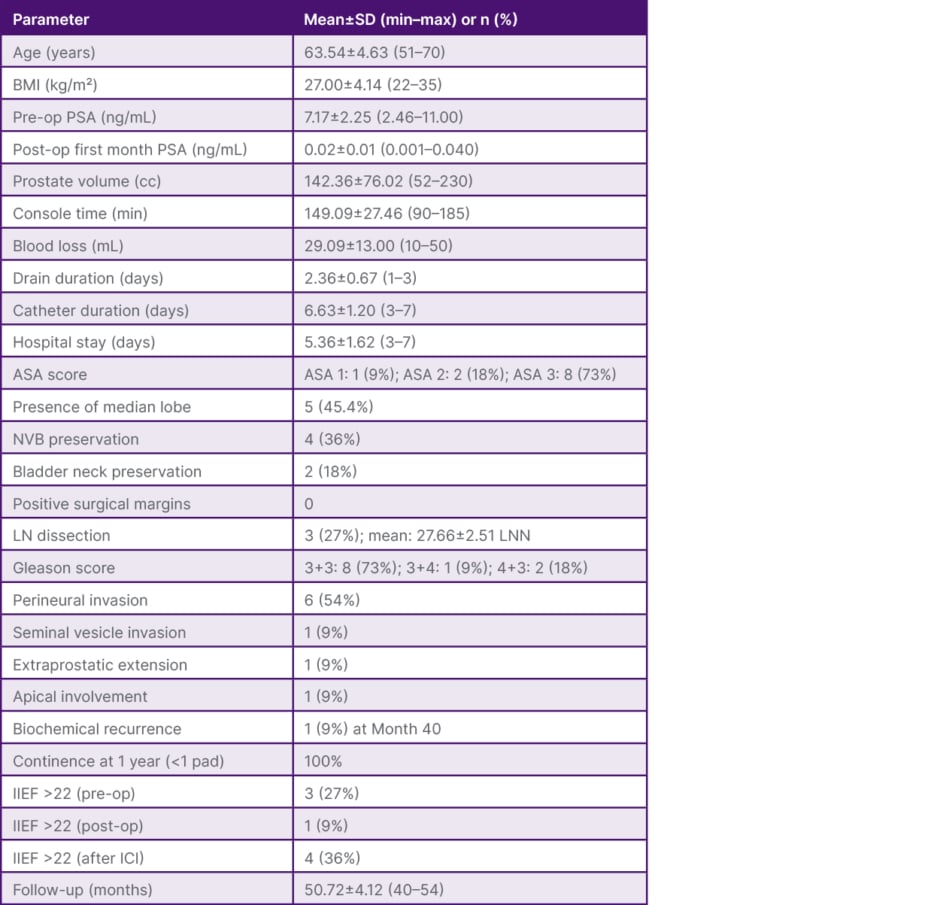
Table 1: Perioperative, pathological, and functional outcomes.
ASA: American Society of Anesthesiologists; ICI: intracavernosal injection; IIEF: Index of Erectile Function; LN: lymph node; LNN: lymph node number; max: maximum; min: minimum; NVB: neurovascular bundle; op: operative; PSA: prostate-specific antigen.
CONCLUSION
RARP in patients with prior TUR-P can be performed safely, with low blood loss, short hospitalisation, and high rates of negative surgical margins. Continence recovery rates are favourable in the medium-to-long term, although erectile function recovery is limited.







