Meeting Summary
Soft tissue fillers treatments historically aimed at correcting signs of ageing such as wrinkles and loss of volume or contour in the face and neck. The ever-expanding range of formulations available on the market have progressively broadened the scope of indications which can be efficiently treated through these minimally invasive modalities,1 including therapeutic applications with targeted volume restoration in specific patient categories, going beyond the scope of anti-ageing and beautification.2,3
Coincidentally, recent research from across disciplines is converging to reveal a far more anatomically organised and functionally dynamic role of facial tissues than initially thought.4,5 These continuous improvements in the understanding of facial anatomy have fostered innovation in the formulation of new hyaluronic acid (HA) gels, aiming to propose products designed to support and fill specific tissue layers, while accompanying and adapting to facial movement through adapted rheological properties.6-7 Therefore, HA fillers have met new clinical needs through customised formulations tailored to specific injection depths, anatomical areas, and facial movement.6,9-13
In this context, clinicians have proposed new injection techniques with dedicated products to support natural facial dynamism.14,15
HA gels have thus gained popularity and evolved from their ’wrinkle filling’ role to become viable alternatives to surgery in therapeutic indications such as facial lipoatrophy, scarring, post-traumatic reconstruction, and facial asymmetry, as well as congenital or acquired facial deformities.2,16,17 Treating these conditions can significantly improve a patient’s quality of life, social interactions, and psychological wellbeing.
During the symposium ‘Beyond Aesthetics’, held at the 2022 AMWC in Monaco and moderated by Patrick Trevidic, Expert 2 Expert, Paris, France, Teoxane’s anatomy, techniques, products (ATP) approach was shown to be a valuable strategy to treat facial asymmetry and remodelling facial volumes after a significant weight loss. Live demonstrations were respectively performed by Paula Rosso, Centro Médico Estético Lajo Plaza, Madrid, Spain, and Sabrina Shah-Desai, Perfect Eyes Ltd., London, UK.
Part 1: How an ATP Approach Can Help to Treat Difficult Cases
Paula Rosso
Any filler injection requires a bespoke treatment approach and a thorough anatomy knowledge to minimise procedural risks and achieve natural-looking results.18,19 The ATP approach implies an injection tailored to each patient, considering their medical and personal history, as well as anatomical specificities related to their age, gender, or ethnicity.20,21 Treating difficult cases, meaning here uncommon facial volume loss or asymmetry, requires a perfect understanding of the facial tissue layers’ arrangement and dynamism. It also requires a proper patient assessment to perform an optimal volume restoration, without adversely affecting facial expressions. In specific anatomical regions (e.g., the midface), adopting a systematic and adapted multilayering treatment approach may be advantageous, and limit overall injection volumes for the same outcome.21
Rosso introduced this session, highlighting that soft tissue fillers injections in aesthetic medicine should not be exclusively devoted to beautification. They may also represent a real option for patients suffering from congenital or acquired conditions, helping them gain self-confidence, and improving their quality of life.
As an example of a difficult case, Rosso reported her own patient case presenting with Moebius syndrome, a rare congenital and non-progressive disease affecting cranial nerves, resulting in facial palsy or bilateral facial paralysis (facial diplegia) and difficulties in eye abduction.22 Facial palsy creates hypertrophic muscle activity on the non-paralysed side of the face, as opposed to atrophic static muscles on the contralateral side. Therefore, the treatment was specific to each side of the face to compensate differences in volume due to unequal muscle activity and thus homogenise facial expressions.
Figure 1A shows the before and after photographs of her patient’s treatment with targeted TEOSYAL® (Teoxane, Geneva, Switzerland) fillers’ injections (as detailed in Figure 1B). The most visible change is in the perioral area, with the elevation of the corner of the mouth. In this category of patients, the treatment not only brings a physical change but induces an emotional change impacting social interactions and overall wellbeing.
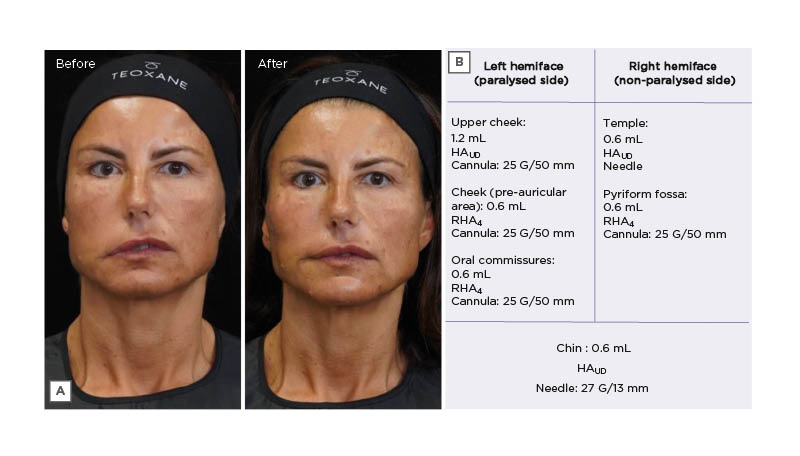
Figure 1: The treatment of a female patient presenting with facial asymmetry.
A) Before and after photographs of a female patient with a Moebius syndrome-associated facial asymmetry, who was treated with TEOSYAL fillers. B) Treatment summary.
HAUD: TEOSYAL PureSense Ultra Deep; RHA4: TEOSYAL RHA 4.
Although this is a rare syndrome, similar facial asymmetry can affect other patient types. Indeed, multiple causal agents may lead to the development of facial asymmetries, including pathological, traumatic, functional, or developmental factors. Overall, the aetiologies of facial asymmetry can be grouped into hereditary factors of prenatal origin and acquired factors of postnatal origin.23
Part 2: Live Demonstration – How to Treat an Asymmetrical Face with Hyaluronic Acid Fillers?
Paula Rosso and Patrick Trevidic
Rosso continued her introduction on asymmetry with the live injection of a 46-year-old female patient presenting a moderate facial asymmetry of congenital origin. As with facial palsy, one side of the face was more hypertonic than the other, while the hypotonic side presented with less wrinkles.
An iterative approach was adopted, adapting the treatment plan depending on the outcomes of each injection step on the overall asymmetry. As recommended for any ‘full face’ treatment, injections were started in the midface to anticipate any impact on other areas of the face.24 In patients who are asymmetrical, two treatment sessions may be required to achieve optimal results: a first one to tackle the asymmetry, followed by a ‘beautification’ session.
Midface
A 25 G/50 mm cannula was used for injecting the deep fat pads of the midface from a single lateral entry point on the zygoma, pinching the skin to ensure deep positioning of the cannula. Injecting the right side only, a highly cohesive and strong projecting filler (TEOSYAL PureSense Ultra Deep [HAUD; Teoxane]) was deposited in these static fat compartments.25 The product was delivered very slowly in small boluses, in the medial and lateral sub-orbicularis oculi fat (mSOOF, lSOOF), and in the deep medial cheek fat (DMCF), injecting 0.6 mL overall on this side to reduce the bilateral asymmetry.
Upper face
Moving to the left side of the face, a ‘gunshot’ technique was performed with a 27 G/13 mm needle in the temple, aiming to put a stiff product very deep to push up the temples and lift up the eyebrow. The technique aimed to touch the bone with the needle and slide it, bevel down, to avoid the deep temporal artery and veins running within the muscle.26 A 0.6 mL volume of HAUD was thus deposited supraperiosteally.
Perioral Area and Lower Face
Pyriform fossa
Progressing to the lower part of the left side, a deep injection of HAUD was performed in the pyriform fossa (i.e., the soft triangle found lateral to the ala of the nose). A bolus (0.4 mL) was deposited in the pyriform fossa with a 25 G/50 mm cannula technique introduced through an entry point on the nasolabial line, advanced first in a superficial plane until the alar fossa before pushing it more deeply to touch the periosteum.
Given that the facial artery (FA) is superficial in that area, the filler should be placed deeply, which is also possible with a needle introduced directly close to the ala of the nose with a perpendicular angle to the skin, until touching the bone with the tip to ensure proper placement.27
Nasolabial folds
The nasolabial folds (NLF) were an important treatment zone in this patient, who showed hyperactivity of the muscles on her left side, exaggeratedly lifting the left upper lip, and emphasising the asymmetry of her facial expressions. Therefore, this treatment step aimed to push down the lifted tissues trough a dedicated left NLF and lower face treatment.
Another volumising but more dynamic filler (TEOSYAL RHA 4 [RHA4; Teoxane]) was selected to slightly fill the patient’s marked expression lines. Despite its high strength score, RHA4 retains a good stretch capacity (i.e., a propensity to deform under facial movement).10 This duality allows it to be placed superficially and moulded after injection to prevent any bump formation.
RHA4 was injected in the left NLF (0.6 mL), introducing a 25 G/50 mm cannula in the immediate subdermis to avoid the FA running very superficially in this area. The entry point was located at the bottom of the nasolabial line to perform a fanning technique, depositing linear threads of product along the fold.28
Perioral area
Afterwards, RHA4 was injected superficially in the marionette lines and oral commissures with a 25 G/50 mm cannula inserted through an entry point in the paramedian chin. A volume of 0.6 mL was injected on each side using a fanning technique, also treating the labiomental line to soften it.
Key vascular dangers of this region were summarised by Trevidic. The inferior labial artery runs underneath the depressor anguli oris and the ascending mental artery lying within the submuscular plane, approximately 6 mm lateral from the midline of the chin, thus advocating the use of cannulas in the superficial plane.29-31
Lips
Moving to the lips, Rosso reminded the audience of the more painful nature of injections performed in this sensitive area. She then emphasised the importance to look at the teeth to establish a treatment plan, as any asymmetry in the teeth means a different support on each side of the mouth.32 The lip treatment step aimed at correcting an asymmetry in the upper lip, which was slightly more elevated on the left side. The injection was performed with a HA filler (TEOSYAL RHA Kiss [Teoxane]) combining high cohesivity and malleability, manufactured with a low HA modification degree, specifically indicated to enhance the contour of the lips.
Entering from the vermilion border and staying very superficial, a volume of 0.5 mL was deposited in micro aliquots, using a 30 G/12 mm needle to correct the asymmetry of the upper lip.
In this area, the main vascular danger is the superior labial artery, which supplies the most lateral third of the half upper lip subcutaneously, then crosses the muscular plane and runs under the mucosa in the in the most medial two-thirds.33,34
Jawline
The finishing touch of this full-face treatment focused on redefining the contours of the patient’s lower face. Both sides of the face were injected, as this final step was an additional treatment of rejuvenation and beautification, rather than mere correction of remaining asymmetry.
In this area, lateral to the mandibular ligament lies the static part of the lower face (i.e., the posterior jawline and the gonial angle), where the masseter directly adheres to the bone without intermediate fat.5
In the lower face, particular attention should be paid to the FA and marginal mandibular branch of the facial nerve. The FA runs deep, just anterior to the masseter where it is easily palpable; hence, it can be avoided by staying in the subcutaneous layer, gently lifting the skin away from the mandible while injecting.35,36 There are two fixed points in the jawline respectively represented by the mandibular ligament in front of the jowl and the pre-masseteric ligament behind the jowl. The contraction of the depressor labii inferioris, depressor anguli oris, and platysma muscles in relation to those fixed points contribute to the disruption of a straight mandibular line during ageing, as they pull the soft tissue downwards, causing a depression zone creating the jowl.12 Therefore, injections should be constrained anterior and posterior to the jowl, whilst the jowl itself must never be filled to avoid worsening this effect.
In this patient, a multilayering technique was used to redefine the mandibular angle and the posterior jawline, recreating a straighter line. First, HAUD was injected deep along the posterior jawline, entering from the jowl with a 25 G/50 mm cannula. This product recreates a structure by acting like an implant. As a second step, Rosso performed a second entry point at the mandibular angle and moved in a more superficial plane to deposit RHA4 on top of HAUD injections, preferring a dynamic and easily mouldable product to prevent the formation of bumps or irregularities at the skin surface. To tackle the patient’s lower face asymmetry, Rosso injected 0.6 mL and 0.8 mL of filler in her right mandibular angle and posterior jawline, respectively, versus 1.2 mL and 0.6 mL on the left side.
Treatment Overview
The main goal of the full-face treatment was to symmetrise bilateral facial volumes. The overall harmony of the face was improved with minimal product quantities, in part due to the multilayering techniques employed in appropriate areas. Before and after 3D photographs taken with a dedicated equipment (using LifeViz® Mini [Quantificare, San Francisco, California, USA]), which can be seen in Figure 2.
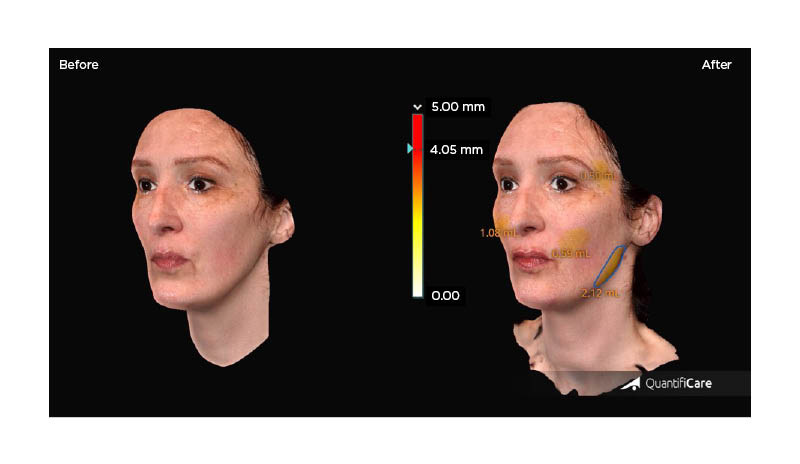
Figure 2: Before and after photographs of Rosso’s patient, who was injected live to showcase the treatment of an asymmetrical face.
The measuring principle is based on a structured light projection. Pre-/post-treatment volumetric changes are presented on the right photograph.
Photographs were taken with the 3D camera LifeViz® Mini and its software, LifeViz® App (Quantificare, San Francisco, California, USA).
Part 3: How to Restructure a Face After a Significant Weight Loss?
Sabrina Shah-Desai
Shah-Desai started the second live injection with a reminder on the important role of aesthetic doctors in restoring their patients’ quality of life; aesthetic medicine not being just about vanity.
She then introduced her 36-year-old female patient, a smoker with a recent history of significant weight loss (8–10 kg) due to work-related anxiety. Her weight loss induced a rapid resorption of her facial superficial fat, which had accelerated the emergence of early signs of ageing, accentuating the bags under her eyes, and giving the impression of a collapsed and sunken face. Consistently, a recent study by Valente DS et al.37 brought forward evidence that a sudden change in body weight causes a change in age perception, potentially making patients appear older than their actual age.
Other patient types may present similar characteristics due to varying conditions resulting in drastic weight loss, such as females who are post-menopausal, patients who have received chemotherapy or bariatric surgery, and patients with HIV presenting facial lipoatrophy (FLA) due to highly active antiretroviral therapy. Interestingly, while volume deflation in the deep fat pads appears to be the primary mechanism that causes ‘pseudoptosis’ of the overlying tissues, weight loss, and HIV-associated FLA manifestations also induce substantial atrophy of the superficial fat (Figure 3).38,39
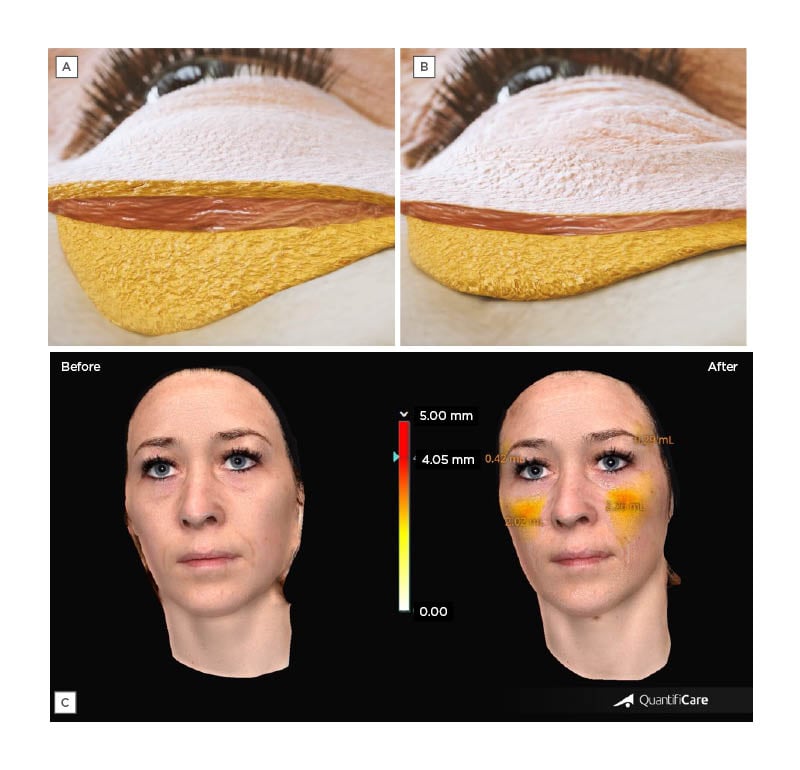
Figure 3: Midface soft tissues after weight loss.
Schematic section of the midface soft tissues A) before and B) after weight loss, illustrating the atrophy of fat layers. C) Before and after photographs of Shah-Desai’s patient, who was injected live to showcase the treatment of facial volume changes after a significant weight loss. Pre-/post-treatment volumetric changes are presented on the right photograph.
Photographs were taken with 3D camera LifeViz® Mini and its software, LifeViz® App (Quantificare, San Francisco, California, USA).
Whenever possible, particular attention must be paid to the cause of the weight loss (e.g., diet, medication, disease) and whether the patient is at risk of regaining this weight (or intends to regain it), as this could impact the treatment plan. Assessing the patient in a frontal view showed the need for midface projection and temple augmentation as these areas presented significant (and slightly asymmetrical) hollowness. The patient also showed prominent eyebags, eligible for infraorbital treatment with fillers, albeit too severe to be fully camouflaged non-surgically. Finally, Shah-Desai asked the patient to smile to visualise her face in a dynamic expression, which showed how her muscles pulled differently on each hemiface, accentuating the asymmetry. The main goal of the treatment was to rebalance the volumes of the patient’s hemifaces, as her right side looked hollower while her right cheekbone had more projection.
Midface
Shah-Desai relied on the patient’s anatomical landmarks to locate her deep fat compartments, drawing a first vertical line down from the lateral orbital rim and a second one following the tear trough (TT) to the mid-cheek groove. The DMCF is found at the confluence of these marks, with the mSOOF and the lSOOF above it, respectively medial and lateral to the vertical line of the face running from the lateral canthus.
HAUD was very slowly injected in the deep static fat pads using a 25 G/38 mm cannula inserted from an entry point in the lSOOF, pulling the tissues up to ensure deep cannula placement. Small boluses of 0.2–0.3 mL were placed supraperiosteally in the DMCF and 0.1 mL in the mSOOF (total volume on the left: 0.4 mL; total volume on the right: 0.5 mL), followed by post-injection moulding. Asking the patient to sit up allowed Shah-Desai to assess the need for additional volume, which was addressed by subcutaneous injections of RHA4, a dynamic filler suitable for accompanying facial movement in the mobile superficial compartments of the midface. Entering from the same entry point, RHA4 was thus injected using a fanning technique (left: 0.6 mL; right: 0.8 mL), while being cautious to not worsen the patient’s temporal hollow.
Upper Face and Periorbital Area
Temple
Injection in the temple started by marking the temporal crest, which can be felt by rolling the thumb in a medial-to-lateral direction over the forehead, until a dip is felt, then marking the lateral orbital rim boundary and the upper border of the zygoma to delineate the visible temple. The audience was reminded of the main vascular dangers, with first the frontal branch of the superficial temporal artery, which can be palpated lateral to the orbital rim.40 As for the deep temporal artery, its anterior branch may be found within the temporalis muscle, when positioning the probe 1 cm superolaterally to the distal end of the eyebrow.41 Finally, a danger zone can also be marked approximately 1–2 cm above the zygomatic arch, where the middle temporal vessels lie.
In this patient, Shah-Desai delivered several retrograde linear threads of filler (TEOSYAL RHA 2 [Teoxane]), 0.5 mL on each side in the deep layer of the inter-fascial plane, using a 25 G/50 mm cannula. The product was then massaged to obtain the desired outcome (i.e., a fuller, but not completely convex temple) to not give the patient a wider look.
Infraorbital hollows
The patient presented visible infraorbital hollows, with marked TT and palpebromalar groove that were accentuated by the bulging appearance of the infraorbital fat. Patients with very large and pronounced eyebags are generally poor candidates for filler injection. The ‘push’ test can be used to evaluate the potential benefits of the procedure. Furthermore, if the aetiology of eyebags is explained by the presence of fluid accumulation rather than prolapse of the orbital fat, treatment with HA fillers may be either disregarded or performed with smaller amounts administered over several treatment sessions to minimise the risk of further impeding the lymphatic drainage.42 45
In this case, it was essential to educate the patient and inform her on the limitations of HA filler injections, as she might have benefit more from a surgical treatment on the long-term. Accessing the area with a 25 G/38 mm cannula, which was introduced laterally, tiny aliquots of TEOSYAL PureSense Redensity 2 (Teoxane) were injected supraperiosteally in her TT and palpebromalar groove (0.5 mL each side) to soften her infraorbital groove with this specifically designed filler.46 Placing the finger of the non-dominant hand above the injected area helped prevent the filler from entering the infraorbital septum. In the TT part of the infraorbital hollows, a little subcision helped detach the cutaneous adhesion of the TT ligament, facilitating cannula gliding along the bone.
Nasolabial Folds
The procedure ended with the treatment of the patient’s NLF. The main danger in this area is the FA, which lies under the zygomatic major muscle and/or just above it in the subcutaneous plane, then becomes very superficial in the upper third of the fold.47-51 As the goal was to inject 0.2 mL of RHA4 into the patient’s left and right pyriform fossa to soften her folds, a cannula entry point was performed at the bottom of the NLF, to advance a 25 G/38 mm cannula superficially before going deep in the upper third to position the filler bolus.
Treatment Overview
Before and after photographs of Shah Desai’s patient can be seen in Figure 3C, with visible changes in surface/volume ratios, as well as an overall appearance improvement, the patient’s face looking less gaunt and less sunken.
Conclusion
Over the past decades, facial aesthetic surgery has lost ground to less invasive procedures that, in the right hands, may provide similar benefits through less traumatic, relatively painless, and less daunting treatments with minimal
social downtime.
Capitalising on their well-established efficacy and safety profile, HA fillers have evolved with dedicated formulations adapted to the specific anatomy and mobility of each treatment area. As a result, a good knowledge of facial anatomy combined with cautious choices of techniques and products achieves natural-looking results with HA fillers which have become a viable alternative to surgery, for both reconstructive and therapeutic indications. In such indications, adopting an ATP approach ensures patient-centred care with safe injection techniques. The ‘A’ for ‘anatomy’ and ‘assessment’ should be the foremost consideration in regard to the patient’s personal and medical history, in addition to general anatomical principles. Most importantly, the psychosocial impact of the treated conditions in this category of patients is often critical, and treatment goals are essential to improve quality of life. A successful treatment may contribute to a more regular life with further social interactions and improved self-confidence, thereby taking part in a global physical and mental healing process.







