BACKGROUND AND AIMS
Early integration of palliative care (PC) is recommended for advanced cancers given its clinical benefits for quality of life and survival, but evidence of its use and the role of provider practice patterns and organizational characteristics in uptake is limited.1 This study examined recent trends of early PC among Medicare beneficiaries newly diagnosed with advanced cancers, and provider- and organization-variation in the receipt of early PC.
MATERIAL AND METHODS
The authors identified patients aged ≥65.5 years newly diagnosed with advanced-stage breast, colorectal, non-small cell lung, small cell lung, pancreatic, and prostate cancers in 2010–2019 with ≥6 months survival and continuous fee-for-service coverage from the linked SEER-Medicare data. Early PC was identified by claims with corresponding diagnosis codes or hospice and palliative medicine provider specialty codes within 90 days post-diagnosis or up to the first hospice admission date (whichever came earlier).2 Treating physicians and corresponding organizations (i.e., Tax Identification Number) were assigned based on the plurality of visits with a cancer diagnosis code within 180 days surrounding cancer diagnosis date. The team described the percentage of patients receiving early PC each year overall and stratified by cancer type. To evaluate the contribution of provider variation in early palliative care use, they first conducted generalized linear probability models with physician- and organization-fixed effects to estimate the proportion of variation in early PC receipt due to between-physicians/organizations variation. The association between several observable physician and organization characteristics and early PC receipt was then estimated. All regression models were also controlled for patient socio-demographic and clinical characteristics.
RESULTS
Among 102,060 patients treated by 19,186 unique providers and 8,039 organizations, the percentage receiving early PC increased from 1.4% to 10.3% in 2010–2019. Although statistically significant increases were observed across cancer types, receipt in patients with prostate cancer was relatively lower compared to pancreatic, small cell lung, non-small cell lung, and breast cancers (Table 1). After adjusting for patients’ characteristics, variation in early PC use between treating physicians and organizations explained 48.2% and 32.7% of the total variation, respectively. Among observable physician and organization characteristics, treating physicians’ early PC referral in the past year (6.76 percentage points; 95% CI: 5.54–7.98) and treating organizations’ employment of hospice and PC specialists (3.18 percentage points; 95% CI: 2.59–3.77) were most strongly associated with early PC receipt.
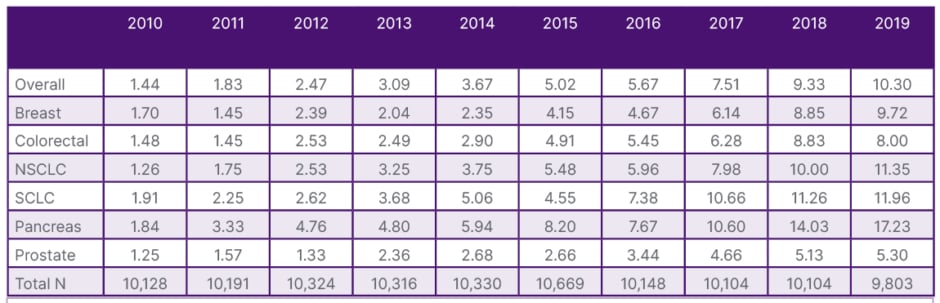
Table 1: Percent of early palliative care receipt among patients with advanced cancers.
N: number; NSCLC: non-small cell lung cancer; SCLC: small cell lung cancer.
CONCLUSION
Despite considerable growth in early PC receipt, utilization remained low in 2019. The large variation between providers and organizations suggests important modifiable provider behaviours and organizational characteristics in early PC use. In particular, education to increase awareness and referral to early PC among physicians and efforts to increase hospice and palliative medicine workforce may be effective tools to promote early PC utilization.







