Abstract
Introduction: Infertility globally poses significant physical, emotional, social, and economic challenges. Despite extensive research on infertility in the general population, there needs to be more understanding regarding its prevalence and effects on healthcare professionals. This article addresses this gap by providing a comprehensive overview of infertility in the healthcare industry, highlighting its unique aspects and implications.
Methods: The search strategy for this literature review yielded 1,323 studies from the following databases: PubMed, Google Scholar, and ScienceDirect. After duplicate removal and screening of the articles using the authors’ inclusion and exclusion criteria, 54 full-text articles were assessed for eligibility. Of these, 21 articles included surveys, cross-sectional, and cohort studies, followed by reviews.
Results: Female healthcare workers, especially emergency physicians and surgeons, face higher infertility risks due to occupational stressors, with 76% of female surgeons utilising assisted reproductive technology for conception, well above the general population. Sleep deprivation from shift work exacerbates infertility, while long hours increase pregnancy complications. Hazards like radiation and chemicals contribute to menstrual disorders and congenital anomalies. Gender disparities persist, impacting career and lifestyle choices among otolaryngologists.
Discussion: Infertility poses challenges for healthcare professionals, with a limited understanding of male infertility. Female surgeons often delay pregnancy due to training, relying on assisted reproductive technologies. Gender differences in divorce and childbirth rates highlight unique challenges females face, including infertility. Long work hours and occupational hazards further complicate fertility issues. Sleep deprivation affects reproductive hormones, impacting fertility across all ages.
Conclusion: Studies indicate that female surgeons face heightened pregnancy risks, underscoring the need for job changes to prioritise parenthood. Career pressures affect female physicians’ decisions to start families, potentially perpetuating gender inequities. Further research on male infertility is crucial for addressing healthcare industry challenges.
Key Points
1. Infertility affects approximately one in six adults, with an estimated one in four female physicians being affected. However, data regarding infertility among male physicians are currently unavailable.2. This systemic review of 21 papers focusses on the issue of infertility among male and female healthcare professionals, aiming to identify the factors leading to infertility since there is a lack of understanding regarding its prevalence in healthcare workers.
3. The impact infertility poses on healthcare workers reveals a lack of adequate knowledge, as well as increased difficulties, especially in female healthcare workers. The findings of this paper suggest the requirement of policy changes to better support pregnant healthcare workers, and address the overwhelming career pressures that negatively affect family planning among healthcare workers.
INTRODUCTION
The healthcare industry is known for its demanding and stressful working conditions. The complex link between job-related stressors and reproductive outcomes among healthcare workers is an intriguing, yet understudied, field of research, despite the demands of this line of work. Infertility globally poses significant physical, emotional, social, and economic challenges. Despite extensive research on infertility in the general population, there is a lack of understanding regarding its prevalence and effects on healthcare professionals. Although studies have shown the general effects of work stress, the precise influence on fertility continues to be a crucial issue requiring investigation. For instance, female surgeons have been reported to have a higher incidence of infertility and pregnancy difficulties than the general population.1 Also, due to their training and early careers, surgeons frequently put off getting pregnant and having children. However, less is known about the risks of infertility and pregnancy difficulties for female surgeons.2 Numerous studies have also shown a higher incidence of highly educated females not having children. In addition, physical stressors such as shift work, prolonged standing, and lifting have generally been linked to a higher risk of spontaneous abortion or preterm birth.3 Therefore, the conflict between biological and professional clocks may be a very significant problem for many female physicians, and may have serious consequences for career advancement and job happiness.4 This article aims to address this gap by providing a comprehensive overview of infertility in the healthcare industry, highlighting its unique aspects and implications.
METHODOLOGY AND STUDY SELECTION
The search strategy for the literature review yielded 1,323 studies from the following databases: Pubmed, Google Scholar, and ScienceDirect. After duplicate removal, and screening of the articles using the authors’ inclusion and exclusion criteria, 54 full-text articles were assessed for eligibility. Of these, 21 articles included surveys, cross-sectional and cohort studies, followed by reviews. Table 1 represents inclusion and exclusion criteria, and Figure 1 represents the identification, screening, and inclusion of studies via databases.
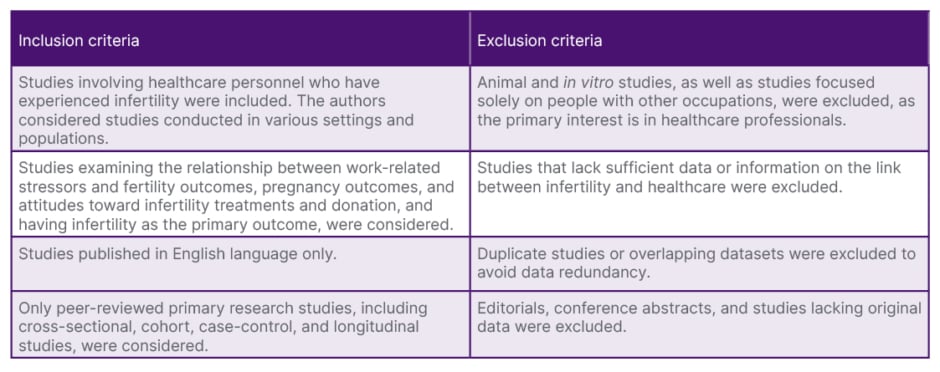
Table 1: Inclusion and exclusion criteria.
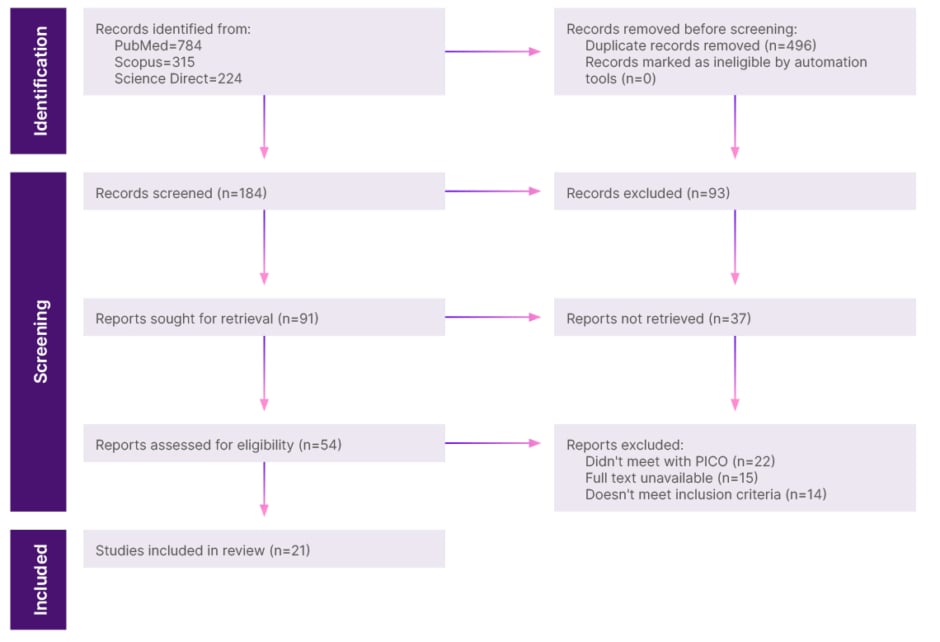
Figure 1: Identification, screening, and inclusion of studies via databases.
PICO: population, intervention, control, and outcomes format.
REVIEW
Data that were consistent throughout the literature, and which were selected to understand the factors that led to infertility in healthcare professionals, proceeded with a common trend: female healthcare workers (especially emergency physicians, plastic surgeons, and nurses) were more drastically affected than male healthcare workers. Female physicians, especially emergency physicians, face various psychological and environmental hazards on a day-to-day basis at their workplace.5 Although physicians reported a pregnancy success rate of 84% for all attempts, female emergency physicians had a much lower pregnancy success rate of only 73%, which created a striking indication of the association between occupational stressors and issues related to fertility.5,6
Male infertility in the healthcare profession was a topic that the staff themselves were quite oblivious to.7 Out of 556 people who took part in the study, 89.39% of them reported that “men feel depressed to be associated with infertility”. This ingrained stigma, irrespective of academic background, creates an environment where people refuse to be educated about the issue. A total of 92.81% reported never taking part in any programmes or training regarding male infertility.7
Like female emergency physicians, female surgeons were reported to suffer from emotional hazards that affected pregnancy, and even impaired their fertility.8 Female surgeons were also reported to have fewer biological children when compared to males in their field, due to the stringent requirements of surgical training and the job itself. Female surgeons showed a higher incidence rate of utilising assisted reproductive technology (ART) to conceive. Of the total number (n=1,021) surveyed, 784 females attempted to achieve pregnancy. Of that number, 32% (n=251) reported difficulty with fertility. Of those reporting difficulty with fertility, 84% (n=210) went on to have a formal fertility workup. Seventy-six percent (n=180) of the females reporting difficulty with fertility used ART to attempt to achieve pregnancy.
Comparatively, in the general American population, infertility was reported in only 10.9% of females, only 11.0% sought infertility treatment, and only 5.2% utilised ART. Remarkably, at least 13% of the infants born to female surgeons were conceived using ART. In addition, female surgeons had 1.4% biological children, which is lower compared to the normal population. The average age at first pregnancy was 33 years, whereas the national average was 23 years. The implementation of ART increased the surgeon’s average age at first birth to 35.4 years. With regard to surgical specialities, otolaryngology recorded the highest rate of infertility (29%), followed by general surgery at 22%, and orthopaedics at 18%.
Complications during pregnancy (such as gestational hypertension and pre-eclampsia), along with complications after the pregnancy (such as musculoskeletal disorders, nonselective Caesarean delivery, and postpartum depression) were much higher among female surgeons when compared to female non-surgeons.
A study comparing female surgeons with the general population reported greater infertility rates and pregnancy-related complications in female surgeons.10 These complications include spontaneous abortion, preterm delivery, fetal growth, and congenital abnormalities. The factors that contribute to this are exhausting working conditions, older age, and the presence of reproductive hazards such as radiation, surgical smoke, and anaesthetic gasses in operation theatres. Therefore, measures must be taken to control detrimental exposures, and female surgeons should be aware of their potential harms.
Rangel et al.2 and Pfennig et al.5 both illustrate that the most common work-related stressor is the sheer amount of time spent at the workplace. A significantly higher risk of infertility with long working hours was associated with females younger than 40 years.4 Females who were experienced with contraceptives also exhibited an increase in their risk of infertility with longer durations of work. Younger physicians exhibited higher levels of emotional exhaustion, depersonalisation, and even a lower personal sense of accomplishment, all of which are detrimental to the emotional status of the physician. Physicians without children in their household had much higher emotional exhaustion and depersonalisation scores when compared to those with children (emotional exhaustion subscale of Maslach Burnout Inventory, and depersonalisation subscales were used to gather the scores). Ages between 36–45 years reported the highest percentage (58.2%) of those who fall under moderate-to-high emotional exhaustion. In contrast, the age group below 35 years exhibited the highest percentages for both depersonalisation and lack of personal accomplishment (51.4% and 77.2%, respectively).11 Hazards such as anaesthetic gas and radiation exposure at the workplace affected 30.4% of the pregnancies, and 8.5% were seeking infertility treatments due to the exposure. Female physicians (no specific subspecialty) showed a higher rate of infertility treatment and miscarriages compared to the general population. This increased rate of infertility and miscarriages was attributed to the lack of personal accomplishment and depersonalisation experienced by them.
Succumbing to the demands of the occupation was also faced with the natural limitation of age. A total of 24.1% of the healthcare professionals from a White background who tried to conceive ended up receiving a diagnosis of infertility.12 This was primarily due to age or diminished ovarian reserve (29.3%), ovulatory dysfunction (29.3%), and male factor infertility (17.2%). It also illustrated how the females mostly underestimated their likelihood of conception at a particularly younger age. According to them, the average estimate regarding the chance of conceiving after a year of unprotected intercourse was 68.3% at age 30, 56.1% at age 35, 33.1% at age 40, and 18.9% at age 45.
Regarding radiology residents, there is an additional hazard of radiation exposure to the fetus during pregnancy.13 Since female physicians represent a minority in the specialty of radiology, programmes may lack formal written policies for fluoroscopy and pregnant workers.
Sleep deprivation is another factor contributing to infertility. Shift work among healthcare workers often involves working at night.14 Hence, the assigned time for sleep coincides with the time of the high circadian alternating signal. This leads to sleep disturbances along with imbalances between the imposed light-dark cycle and endogenous circadian systems. Improper sleep among female shift workers causes pregnancy loss, amenorrhoea, anovulation, and failed embryo implantation. This is thought to be because lack of sleep suppresses the production of melatonin, and excessive hypothalamic-pituitary axis activation. Changes in gonadotropin and sex hormone secretion have also contributed to infertility. In middle-aged and older males, sleeplessness has been associated with decreased testosterone levels.
A cross-sectional study conducted in Japan, among female physicians, demonstrated the relationship between pregnancy complications and long working hours.15 It was found that females who worked 71 hours or more per week had a three-fold greater risk of experiencing threatened abortion in comparison to those who worked 40 hours or less per week. The risk of experiencing preterm birth in females working 51–70 hours was 2.5 times higher, whereas the risk is 4.2 times greater in those working 71 hours or more.
Regarding the emergency department, it was noted that the frequency of menstrual disorders in clinical staff was greater than that of administrative workers.16 The differences were quite significant, with contributing factors including the physical and emotional exhaustion that comes with the field, along with exposure to hazards such as radiation, anaesthetic gasses, certain chemicals, and drugs.17
There have been increased incidences of congenital anomalies amongst healthcare workers in comparison to non-healthcare workers.18 Increased risk of fetal death is associated with exposure to sterilising agents (glutaraldehyde and ethylene oxide) and, rarely, antineoplastic drugs.
Three research investigations examined how exposure to antineoplastic drugs impacts the likelihood of miscarriage, stillbirth, or both among nurses.19-21 Among the studies focused on miscarriage, one indicated a notable increase in risk linked to antineoplastic drug exposure during pregnancy. Lawson et al.’s19 stratified analyses revealed that this heightened risk specifically pertained to early miscarriages rather than late ones. Similarly, neither of the studies investigating the risk of stillbirth identified a significant correlation with this type of exposure. No association between stress, and fetal death or congenital abnormalities was found. Females working for more than 40 hours per week have a higher risk of irregular menstrual cycles. However, no relationship with the length of the menstrual cycle was found. There has been a small risk of miscarriage associated with longer working hours, and fixed night work. Studies on paternal exposures are rare.
Another study was conducted to identify differences in career and lifestyle factors between male and female otolaryngologists.16 It was found that only 59.9% of the females, from the sample in the study, had children, with the average number of children being 2.4. In males, on the other hand, 82.5% had children with an average number of children being three. Furthermore, females with more children reduced their work hours.
DISCUSSION
Infertility has become a challenge that has affected the wellbeing of the general population. The effect of infertility on healthcare professionals is yet to be understood. In a few studies, it has been revealed that there is generally a lack of adequate knowledge about, and a negative attitude towards, male infertility.7 The participants were medical students or healthcare professionals from Bangladesh, who were surveyed anonymously on their knowledge, attitude, and perception regarding male infertility. Among the 556 participants, 49.82% did not have a good knowledge of male infertility, and nearly 60.79% had negative attitudes regarding male infertility. Young (23–26 years) healthcare professionals and medical students were more likely to have good knowledge than others (odds ratio: 1.81; 95% CI: 1.099–2.988).7 It has been revealed that female surgeons were more likely to delay pregnancy due to training, utilise ART, and experience pregnancy difficulties.8 Compared to their male coworkers, females are more likely to stay single, get divorced, and have fewer or no children. The observed gender variations in divorce rates and childbirth rates may reflect the unique difficulties females encounter, such as infertility.16
Of female otolaryngologists, 80.4% were married at the time of the survey, compared with 87.3% of males. Females were more likely to be divorced than male otolaryngologists (8.6% versus 2.9%; P=0.001). Males (among those who were spouses or partners) had more children (mean: 3.0 versus 2.4; P<0.001), and were less likely to be without children than females (P<0.001).16 Reducing the number of hours that pregnant doctors work was significantly hampered by a lack of institutional support, which included insufficient maternity leave and difficulty in hiring substitute staff. Pregnancy problems were more likely for surgeons who worked more than 12 hours a day, averaging over a week during their pregnancies.15 It has been suggested that night shifts, long workdays, prolonged standing, and a heavy physical workload hurt the success of conception and pregnancy.4 However, there is little evidence of lengthy work hours affecting fertility. There are occupational risks due to various exposures in different specialties.5 Workplace risks include night shift work, organic solvents, and heavy metals, which may negatively impact a person’s ability to conceive. Infertility, menstruation problems, and subfertility were shown to be more common in this population.10 Dysmenorrhoea is more common among nurses, and has a significant correlation with ageing and lower BMI.12 Burnout harms both physical and mental health, as well as reproductive health.11 Moreover, working females who use contraceptives may experience a range of obstetrical and gynaecological issues. According to the current investigation, their long workdays put them at risk for infertility.4 Infertility across all ages is affected by quality, timing, and sleep duration.14 Lack of sleep affects the levels of reproductive hormones, which are essential regulators of both male and female fertility.
LIMITATIONS
Although the authors’ review provides valuable insights into the challenges faced by healthcare professionals dealing with infertility, there are some limitations to be acknowledged. During the search, there was little to no evidence of male infertility among physicians, along with a lack of interventions for infertility among male healthcare professionals.7,16 Another significant area for improvement in this review was the reliance on existing research and surveys that may have been conducted on relatively small samples of healthcare professionals.5,7
Recall biases on pregnancy-related details can manifest within both childbearing and non-childbearing healthcare professionals.2 Questionnaire-based bias may arise when participants engage in self-reporting, potentially leading to hesitancy in responses, or difficulty comprehending the posed questions.2,5 Various studies included in the review consist of unmatched survey times, lack of longitudinal data, challenges in generalising findings due to differences in working conditions and cultural factors, potential influences from age-related factors and healthy worker survivor effects, reliance on limited data sources, and a lack of exploration into long-term trends or associations over time.12-14,17 Additionally, gaps in knowledge or the introduction of new information on specific topics, either not covered during the study or introduced post-study, can impact data accuracy.
CONCLUSION
Existing studies emphasise how childbearing surgeons are more likely to experience serious pregnancy difficulties and infertility, so the increasing prevalence of infertility and pregnancy-related risks highlights the necessity for a change in their jobs to prioritise pregnancy. Furthermore, female physicians claimed that pressures related to their careers were affected when they had children, and caused significant changes to their career paths to make room for starting a family, and becoming a parent. So, these findings imply that worries about starting families and having children among female doctors may contribute to lingering gender inequities and attrition, and they point to a possible key area for future policy change. Moreover, additional research and interventions about male infertility are required to address the unique challenges and implications of infertility within the healthcare industry.







