Laparoendoscopic single-site surgery (LESS) represents any minimally invasive intra-abdominal surgical procedure performed through a single incision/location and aims to reduce the already limited invasiveness of conventional laparoscopy even further, to offer not only a better cosmetic result, but also to potentially reduce post-operative pain and offer a quicker convalescence.1
After >900 laparoscopic radical prostatectomies (RPs) performed since 2001,2,3 in 2009 we accomplished our first LESS RP. It cannot be denied that some limitations were encountered. Placing several parallel instruments in a single multichannel port made triangulation more difficult, reducing proper tissue retraction and resulting in clashing of the laparoscope with instruments and a limited operating field. These difficulties were particularly disturbing during the reconstruction phase, when performing vesicourethral anastomosis. Some authors suggested the use of bent, articulated, and different length instruments (i.e. obese and paediatric equipment).4,5 We have personally always adopted an extra 5 mm port placed in the left fossa iliaca.6 As a matter of fact, a recent multi-institutional study7 confirmed that the use of an additional port occurred in 23% of the cases.
In order to overcome these limitations, we presented our preliminary experience (IDEAL Phase I)8 with robotic-LESS RP performed with the da Vinci® single-site robotic platform (Intuitive Surgical, Sunnyvale, California, USA), a semirigid operative system with that incorporates a multichannel single port that accommodates two curved robotic cannulas. The master-slave software automatically exchanges the master-slave controls allowing the surgeon at the console to control the tip of the instrument with their right hand at the right side of the surgical field and the opposite for the left.
At this stage, not all surgical instruments have the wrist at the tip like conventional robotic da Vinci instruments (Intuitive Surgical, Sunnyvale, California, USA) do. We suggest a handmade port-access by combining the single-site multichannel Alexis® wound retractor, and the laparoscopic cap (Applied Medical, California, USA) (Figure 1). The robotic instruments adopted were two endo-wrist needle drivers and a hook, along with the Filbloc® barbed suture (Assut, Rome, Italy) (Figure 2).
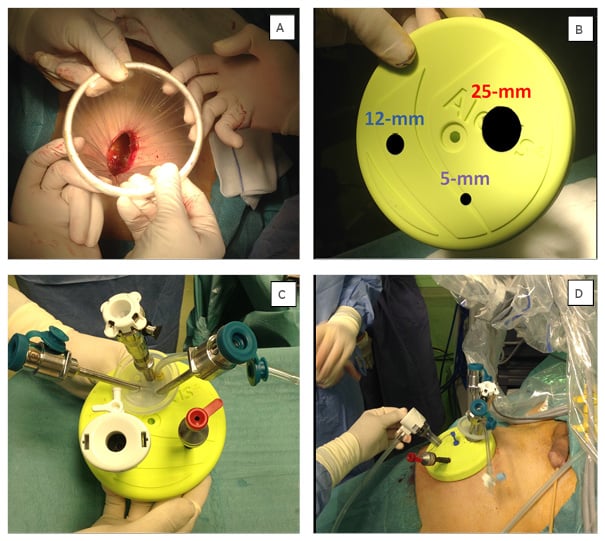
Figure 1: Handmade port-access.
A) We performed a 5 cm paraumbilical incision and introduced the Alexis wound retractor.
B,C) We inserted, through 3 entry-holes made in the laparoscopic cap (25 mm, 12 mm, and 5 mm), the multichannel port and a 12 mm and a 5 mm trocar. D) Finally we plugged the handmade ports and docked the robot.
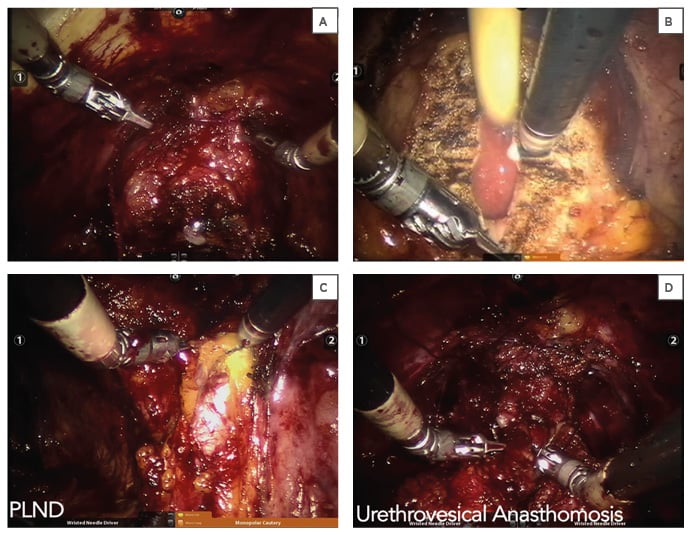
Figure 2: Surgical Steps.
A) Dorsal venous complex (Santorini’s plexus) suture, B) bladder-neck dissection, C) extended pelvic lymph node dissection (PLND), D) urethrovesical anastomosis.
Operative time for the very first procedure was 310 minutes and dropped to 210 minutes by the third case. The assistant was able to simultaneously use two different laparoscopic instruments and easily apply 10 mm clips. A robotic needle-driver was used as a grasper in order to confer more traction and firmness to tissue. There was no need to convert to hybrid robotic-LESS (2 ports) or a standard robotic-approach (5–6 ports) in the three surgeries performed. Mean blood loss was 150 mL and there were no intraoperative or postoperative complications. Patients were discharged on the 3rd postoperative day and their catheters were removed on the 7th postoperative day following urethrocystogram.
This Phase I IDEAL study demonstrated that a pure Robotic-LESS-RP performed with the new dedicated platform in combination with a handmade port is feasible and safe, eliminates instrument crossing, and offers superior ergonomics for both the robotic surgeon and the bedside assistant, whilst the needle-driver tip articulation significantly facilitates suturing.
The lack of endo-wrist technology applied to other instruments (scissors and forceps) requires improvement.








