BACKGROUND
In 40–70% of patients referred to a haematologist for the evaluation of an increased bleeding tendency, no diagnosis can be found after extensive laboratory testing.1 These patients are classified as having a bleeding disorder of unknown cause (BDUC). Their bleeding phenotype resembles that of patients with known (mild) bleeding disorders, including platelet function disorders.2 Currently available laboratory haemostasis tests are unable to diagnose these patients.3 Therefore, the aim of this study was to investigate the underlying pathophysiological bleeding mechanism in patients with BDUC by using a microfluidic assay to identify shear-dependent primary haemostasis defects.4
METHODS
Data from the ProBe-AHP cohort were analysed. In this cohort, patients referred to the haematologist for the analysis of an increased bleeding tendency were included. This study was previously described in more detail.5 Patients with BDUC who had an increased International Society on Thrombosis and Haemostasis – Bleeding Assessment Tool (ISTH-BAT) score, as well as normal von Willebrand factor levels, light transmission aggregometry, and ATP release, were selected from this cohort. Shear-dependent platelet adhesion, activation, and aggregation were assessed using microfluidic analysis of shear-dependent collagen only, and/or collagen with tissue factor induced whole blood thrombus formation at 37°C.6,7
RESULTS
In 26/48 (54%) selected patients with BDUC, who had a mean ISTH-BAT score of 10, abnormal shear-dependent platelet function was observed compared to reference ranges based on measurements in 49 healthy controls. A combination of lower platelet adhesion, lower integrin activation, lower phosphatidylserine exposure, and/or lower P-selectin expression was seen in these patients (Table 1). Additionally, the visually assessed morphology, contraction, and multilayer scores were impaired in 5/48 patients with BDUC. Fibrin formation on a collagen Type I spot co-coated with tissue factor showed no statistically significant difference between patients with BDUC and healthy volunteers.
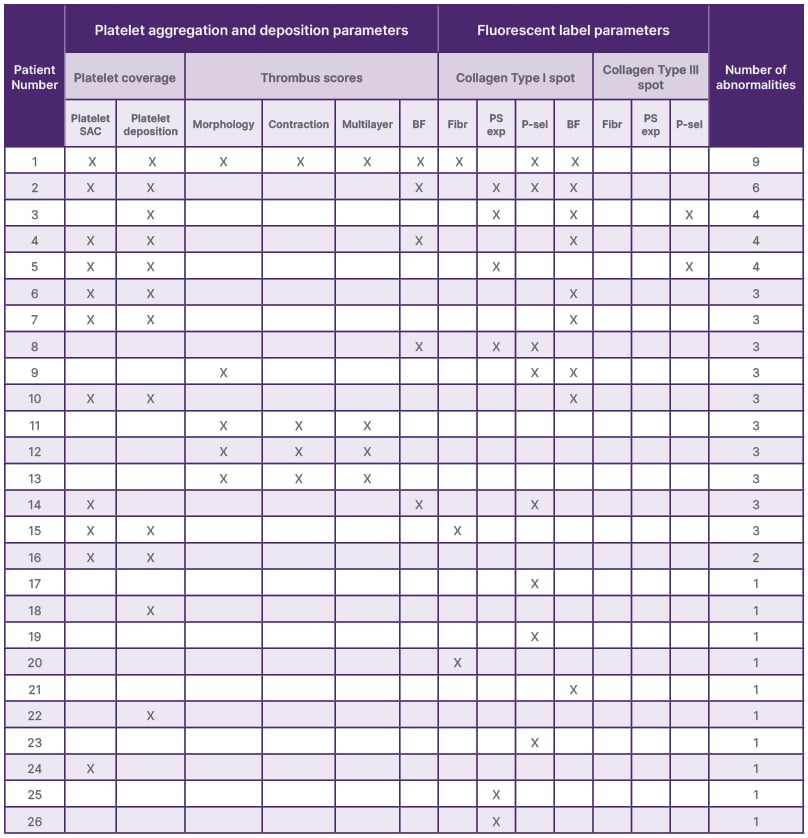
Table 1: Overview of the abnormalities found per parameter* in patients with bleeding disorder of unknown cause (N=48).
*Number of abnormalities in platelet SAC: 11; platelet deposition: 12; morphology score: 5; contraction score: 4; and multilayer score: 4. Number of abnormalities on collagen Type I: BF: 5; Fibr: 3; PS exposure: 6; and P-selectin: 8. Number of abnormalities on collagen Type III: BF: 9; Fibr: 0; PS exposure: 0; and P-selectin: 2. No abnormalities found in 22 patients with BDUC.
BDUC: a bleeding disorder of unknown cause; BF: brightfield; Fibr: fibrinogen; P-sel: P-selectin; PS exp: phosphatidylserine exposure; SAC: surface area coverage.
CONCLUSION
Results from this study show that microfluidic analysis of whole blood thrombus formation under shear can identify shear-dependent platelet function defects in 54% of patients with BDUC, in whom light transmission aggregometry, ATP-release, von Willebrand factor activity, and antigen levels are normal.







