Abstract
Cocaine-induced leukoencephalopathy is a rare neurological condition usually associated with substances used to adulterate cocaine. A common adulterant of cocaine includes levamisole, an anti-helminthic agent, causing pathologies including vasculitis, agranulocytosis, and, in rare cases, leukoencephalopathy when ingested. Here, the authors present a comprehensive analysis of a cocaine-induced leukoencephalopathy case with the likely presence of levamisole. The patient, a 31-year-old male with an unknown past medical history, presented to the emergency department with seizure-like activity, stiffness, and posturing. Signal abnormalities found in imaging can be seen in the setting of acute cocaine-induced leukoencephalopathy and other metabolic etiologies. The patient was admitted to the neurocritical care unit for management of toxic leukoencephalopathy, acute respiratory failure with hypoxia, non-traumatic rhabdomyolysis, aspiration pneumonia, acute renal failure, and hypertensive emergency. After a 12-day hospitalization, the patient improved towards baseline and continued follow-up for further management. The case study exhibits the importance of early recognition and treatment of cocaine-induced leukoencephalopathy, the possible impacts of adulterated cocaine, the clinical outcomes of induced leukoencephalopathy, and the poor clinical outcomes without prompt intervention. Also included is the argument for levamisole testing when suspected and the use of intravenous methylprednisolone in these cases versus previously described management with methylprednisolone.
Key Points
1. Cocaine-induced leukoencephalopathy is a rare and potentially lethal adverse outcome of cocaine ingestion. This article discusses the use of high-dose IV methylprednisolone and its success in this case, adulterant considerations with testing and treatment, and future indications regarding testing and treatment of suspected cocaine-induced leukoencephalopathy.
2. A case study of a patient diagnosed with cocaine-induced leukoencephalopathy, its unique management, and considerations for similar cases.
3. Methylprednisolone has had mixed results in the treatment of cocaine-induced leukoencephalopathy in other case reports. Clarifying the dosing of intravenous methylprednisolone may be of benefit to patients in the future, especially if suspicion of Levamisole adulteration is present.
INTRODUCTION
Cocaine-induced leukoencephalopathy is a rare neurological condition usually associated with substances used to adulterate cocaine. A common adulterant of cocaine includes levamisole, an anti-helminthic agent causing pathologies including vasculitis and agranulocytosis when ingested .1 Levamisole is thought to be used to add weight and volume, with possible potentiation of the effects of cocaine.2 With over five million Americans using cocaine and an estimated 70% of cocaine in the United States being adulterated with levamisole, this poses a serious health burden.1 Other known adulterants of cocaine include the historical use of local anesthetics, and more recently phenacetin, amphetamines, methamphetamines, and psychoactive substances.3 These substances commonly amplify the toxic effects of cocaine, creating more serious health risks.
Patients with toxic leukoencephalopathy usually present with confusion, behavior changes, extrapyramidal symptoms, generalized motor deficits, and unresponsiveness, which can result in death. The case studies published detailing cocaine-induced leukoencephalopathy usually result in the patient making a full recovery when identified and treated promptly.4-6 This pathology has been compared to spongiform encephalopathies, with fluid entrapment within vacuoles within the myelin lamellae that surround the axons and are represented on imaging by the expansion of brain involvement, though clinical improvement is being made.4 Below is a detailed report of a patient’s hospital course after the use of suspected adulterated cocaine and its 12-day management.
CASE
We present a case of suspected cocaine-induced leukoencephalopathy. The patient, a 31-year-old male with an unknown past medical history, presented to the Emergency Department (ED) after being found with altered mental status in his vehicle. On arrival to the ED, the patient was ill-appearing and could not protect his airway and was therefore given naloxone and intubated, with seizure-like activity occurring, with stiffness, posturing, and incontinence. On admission, his vitals included a heart rate of 56 beats per minute, temperature of 98.1 °F (36.7 °C), respiratory rate of 16 per minute, oxygen saturation of 97%, and blood pressure of 210/110 mmHg, indicative of hypertensive emergency.
His neurological exam yielded a Glasgow Coma Scale (GCS) score of four. There were roving eye movements with no gaze deviation, which improved throughout his hospital stay. The cough reflex was intact when elicited. Brachioradialis deep tendon reflexes included a 3+ response bilaterally, with a positive Hoffman sign bilaterally. The left lower extremity deep tendon reflex was 3+, with a crossed adductor reflex present. The patellar reflex in the right lower extremity was 2+. An upgoing Babinski reflex was present in the left lower extremity and absent in the right lower extremity. The general sensory response included intermittent grimacing to proximal painful stimuli to the face and trapezius muscle.
The patient was admitted to the neurocritical care unit for management of an initial working problem list, including toxic leukoencephalopathy as the primary problem, acute respiratory failure with hypoxia, status epilepticus (resolved in ED), non-traumatic rhabdomyolysis, aspiration pneumonia, hypertensive emergency, and acute renal failure. The ED review of symptoms for this patient was not received, but was negative for signs of trauma, with normal heart and abdominal sounds. The patient’s girlfriend denied observation of fever, chills, nausea, and vomiting.
Additional history taken from her was consistent with the patient likely experiencing a seizure in his car after ingestion of cocaine. A previous stay of the patient revealed no history of seizures. His serum CK level was later found to be elevated at 26,369 with concern for rhabdomyolysis, another sign that is associated with seizures. The patient’s status epilepticus resolved after Lorazepam and a Levetiracetam load of 4.5 g, followed by 750 mg twice daily during stay.
Labs ordered for the patient included a urine drug screen (UDS), metabolic and blood panels, and inflammatory markers, with the UDS positive for cocaine and negative for other illicit drugs tested on a basic UDS. Cardiac exam included auscultation negative for rubs, murmurs, or gallops. A transthoracic echocardiogram revealed a normal ejection fraction of 52%, with no wall motion abnormalities and normal systolic function.
CT-Angiography (CTA) of the chest was obtained on day one of admission and resulted in bilateral upper and lower lobe-dependent opacities concerning for aspiration. Based on these findings, periodic chest X-rays were ordered to monitor progression. CTA of the abdomen was suggestive of an indeterminate left renal lower pole <1 cm lesion. CTA of the head, neck, and pelvis reported no acute abnormalities. Chest X-ray from day five demonstrated a small left pleural effusion with mild interval improvement in hazy opacities in the right lower lung field and ideal endotracheal tube placement.
An MRI of the head conducted on Day 2 revealed bilateral hemispheric diffusion restriction predominantly involving the subcortical and deep white matter, sparing the subcortical U fibers. Signal abnormalities, diffusion restriction within the cerebellar hemispheres, and a single small nodular focus of diffusion restriction in the left cingulate gyrus were also found. These signal abnormalities would not usually present in status epilepticus and would be highly atypical in infectious etiology, further narrowing the authors’ differential diagnosis towards cocaine-induced leukoencephalopathy and other metabolic etiologies.
An MRI of the head conducted on Day 5 is shown below in Figure 1 A–B, demonstrating an interval increase in the extent of white matter signal abnormality, likely representing the evolution of toxic leukoencephalopathy. Evolving small late-acute to early subacute infarcts in the left cingulate gyrus and bilateral cerebellar hemispheres are thought to be due to cocaine-induced vasospasms. Hypoxic ischemic injury could have contributed to these findings, but is less likely due to the lack of additional cortical and gray matter involvement.
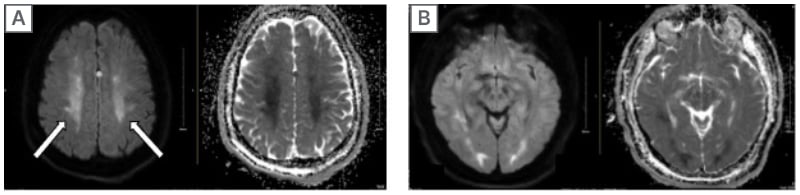
Figure 1A–B: MRI head with and without contrast on Day 5.
Figure 1A and B show bilateral hemispheric diffusion restriction predominantly involving the subcortical and deep white matter with sparing of the subcortical U fibers, as well as signal abnormality and diffusion restriction within the cerebellar hemispheres. A single small nodular focus of diffusion restriction in the left cingulate gyrus is also shown.
Management of this patient’s cocaine-induced leukoencephalopathy included empiric intravenous (IV) methylprednisolone with a ketamine drip due to clinical suspicion and lack of convincing alternative diagnoses. The patient’s systolic blood pressure goal was <140 mmHg, and oxygen saturation was stable, being above 95% while intubated and status-post intubation on Day 10.
The patient’s hypertensive emergency was managed with amlodipine and hydrochlorothiazide given daily during a hospital stay. Management of aspiration pneumonia due to positive findings on chest CT, chest x-ray, and CBC with leukocytosis was managed with vancomycin and piperacillin/tazobactam injection on Days 1-2, ampicillin sodium/sulbactam sodium on Days 2-6, and piperacillin/tazobactam injection on Day 12 through the discharge course. His acute renal failure and rhabdomyolysis improved during stay with a fluid goal of 100 mL/hour, and CK and creatinine levels returned to normal values by the end of stay.
The patient’s acute respiratory failure with hypoxia was managed with intubation upon admission for airway protection and placed on continuous positive airway pressure. Sedation was controlled with midazolam and ketamine, with ketamine boluses administered for agitation episodes. Nicardipine was given as needed for blood pressure control due to previously prescribed amlodipine and hydrochlorothiazide for hypertension management that was continued through his hospital stay. Additional medications for acute altered mental status management and agitation were as needed: lorazepam, IV thiamine, and 50 mg of quetiapine twice daily. For pain management, the patient was given oxycodone, gabapentin, and fentanyl.
FOLLOW-UP AND OUTCOMES
On Day 10, the patient was extubated and placed on bilevel positive airway pressure, continuing to show improvement in his respiratory status. He experienced no additional seizure activity after his initial event. After a 12-day hospitalization, the patient improved towards baseline, being alert and oriented, ambulatory without assistance, and without complaints of pain or shortness of breath. The patient returned for follow-up for further management of baseline hypertension and post-hospital assessment.
DISCUSSION
Clinical Course
The neurologic complications of cocaine overuse are many, with the most common being strokes, seizures, and cognitive deficits.7 However, cocaine-induced leukoencephalopathy is a rare problem occurring most likely due to adulterated cocaine, namely levamisole. Common MRI findings are diffuse white matter involvement with sparing of the subcortical U fibers, T2 signal abnormalities, and diffusion restriction; in this case, it was present in the left cingulate gyrus. Subcortical U fibers are also called short association fibers and connect adjacent gyri, located either within the cortex or immediately deep in the subcortical white matter.8 Due to their myelination and good blood supply, they tend to be affected last in chronic ischemic disease unless in the setting of a direct attack on oligodendrocytes, such as leukoencephalopathy.8
Repeated MRI brain imaging was performed to compare white matter evolution, which is important in monitoring the progression of hyperintensities. Other differential MRI findings of brainstem or cerebellar involvement point more toward leukoencephalopathy due to heroin use.9 Aside from MRI findings, complications of cocaine-induced leukoencephalopathy include confusion, behavior changes, extrapyramidal symptoms, generalized motor deficits, and unresponsiveness, which can result in death.
Comparing Management
While the patient was in the Neuro-ICU, empiric IV methylprednisolone was initiated to reduce inflammation, and levetiracetam was initiated for status epilepticus present upon arrival. Discontinuation of the offending agent is also important for the progression of treatment. In this case, a 12-day hospital stay resulted in this patient’s return to baseline due to medical stabilization and treatment with removal of the offending agent. One similar case of cocaine-induced leukoencephalopathy from 2015 reported that the patient, after stabilizing from initial treatment, was readmitted because of further cocaine use, and an MRI showed prominent worsening of the patient’s lesions.9
One controversial aspect of cocaine-induced leukoencephalopathy is the management of the clinical disease due to uncertainty on what management is best for patients undergoing this disease course. The authors’ patient received a daily IV of methylprednisolone 1 g for 5 days. Other cases with similar presentations, however, have shown patients receiving different doses of steroids or different treatments altogether. For instance, some professionals suggest higher doses of steroids, such as methylprednisolone 1 g, can result in the death of these patients,10 with possible benefit of lower doses of 250 mg to allow recovery. Two similar cases of cocaine-induced leukoencephalopathy in a 31-year-old female and a 19-year-old male sadly resulted in their deaths despite undergoing treatment with boluses of 1g methylprednisolone.11 This may suggest dosing changes based on clinical parameters to be advantageous for patient recovery, with these parameters not yet established.
An alternative route is a more conservative approach. One case presented with a 58-year-old male who received supportive care once the infectious etiology was ruled out.12 This approach showed symptom resolution with a hospital length of stay like our patient. Another conservative approach for a 55-year-old male did not end in recovery. His treatment consisted of CoQ10, vitamins E and C, and levetiracetam for seizure prophylaxis.13 While this patient partially recovered, he did not regain full cognitive function, which may allude to more aggressive treatment with steroids, as with our patient, as is the treatment of choice. This would be especially true if Levamisole is detected.
Management and Diagnostic Considerations
Due to the rarity and inconsistent clinical presentation of cocaine-induced leukoencephalopathy, it is essential to consider the factors potentially causing the wide array of symptoms. Cocaine used by patients is often adulterated with substances such as levamisole, diltiazem, local anesthetics, and hydroxyzine.14 Levamisole causes central nervous system vasculitis and reversible leukoencephalopathy by interfering with mitochondrial function and oxidative stress pathways, exacerbating neuronal damage.14 The combination of levamisole and cocaine can result in the formation of aminorex, an amphetamine-like drug, leading to synergistic effects. This combination can have irreversible effects on neuronal receptors, eliciting a stronger response than if either drug were used alone.14 As a result, the composition ratio heavily influences the symptoms experienced by the user.
In any suspected case of cocaine-induced leukoencephalopathy, further testing to evaluate the concentration of levamisole may be necessary to guide treatment regimens, typically including pulsed IV methylprednisolone. This case is notable because the patient was treated with high-dose methylprednisolone, which in combination with removal of substance exposure is aligned with treating primary levamisole intoxication. The patient’s rapid improvement toward baseline may be an indication that the cocaine ingested by the patient had a higher concentration of levamisole, making the treatment effective. In a similar case presentation, a patient was being treated with only supportive care and was not improving.15 After the use of methylprednisolone, the patient’s mental status improved, and was subsequently extubated 10 days later, similarly to the authors’ patient. These scenarios underscore the potential benefit of levamisole testing, which uses sulfate or glucuronide levels in the urine to determine the appropriate treatment approach. Further research would benefit from clarifying whether levamisole-induced leukoencephalopathy responds to dose-based methylprednisolone, and if identifying levamisole amounts would steer clinical decision making regarding these treatment options.
Differential Considerations
Though negative in the authors’ patient, in patients with heroin-induced leukoencephalopathy, similar MRI findings can be noted when compared to cocaine-induced leukoencephalopathy. A case study analyzed the MRI findings of three patients abusing heroin, cocaine, and cannabis, and a symmetrically increased T2 and T2-FLAIR signal intensity of the cerebellar and posterior cerebral white matter and sparing of subcortical U fibers.16 Although imaging and lab findings are similar in both diagnoses, they significantly differ in pathophysiological disease progression. Patients with heroin-induced leukoencephalopathy typically present with a more progressive spongiform type of encephalopathy with the presence of intracytoplasmic vacuoles. Those affected by cocaine-induced leukoencephalopathy have a more demyelinating pattern.17 These patterns could influence disease progression and prognosis, respectively. Many factors must be taken into consideration when deciphering between polysubstance abuse leukoencephalopathy and purely cocaine-induced leukoencephalopathy, for reasons including increased adulterant use in illicit drugs, drug–drug interactions competing for common neuron receptors, and the method of use, since inhalation versus intravenous intake causes neuronal receptor concentration discrepancies.
Another differential to consider in this patient’s hospital course is hypertensive leukoencephalopathy. Hypertensive leukoencephalopathy primarily affects the white matter of the brain, which is usually due to a sudden and severe elevation in blood pressure. It’s often part of a hypertensive emergency and can be reversible when treated promptly. Similar signs present in this case that were present in our patient were his altered mental status and seizure activity. As explained in the case presentation, however, this was less likely due to imaging findings. Regardless, blood pressure goals were maintained as a part of the patient’s treatment protocol.
Limitations
This case study is inherently limited by its observational and anecdotal nature, which restricts the generalizability of its findings. The treatment approach used, while clinically guided, requires further investigation to establish broader applicability and efficacy. Although levamisole was strongly suspected as the adulterant in the patient’s cocaine use, this was not confirmed through toxicological testing, leaving room for uncertainty regarding the specific causative agent. Additionally, the absence of certain clinical data limits the authors’ ability to fully understand the underlying pathophysiology and clinical trajectory in this case. Regardless, we believe the novel treatment and the need for additional, more specific testing would be of benefit in future cases.
CONCLUSIONS AND RECOMMENDATIONS
The case study exhibits the importance of early recognition and treatment of cocaine-induced leukoencephalopathy, the impact of levamisole-adulterated cocaine, the clinical outcomes of induced leukoencephalopathy, and the poor clinical outcomes without prompt intervention. This patient presented with altered mental status and diagnoses of cocaine-induced leukoencephalopathy, hypertensive emergency, and acute respiratory failure. The combination of intubation with IV methylprednisolone and levetiracetam and discontinuation of the offending agent offered a swift recovery to baseline for this patient. Had the recognition of cocaine-induced leukoencephalopathy not been so expeditious, this patient’s prognosis would likely be more severe. Therefore, early diagnosis and recognition are vital in treating this condition.
A larger understanding of adulterated cocaine complications will not only advantage treatment and management protocol but will help the general population through a greater appreciation of the negative outcomes of illicit cocaine use. There is still more information needed to determine the best course of action for the treatment of suspected cocaine-induced leukoencephalopathy, but this study highlights possible benefits of IV methylprednisolon along with supportive care, along with the potential benefit of levamisole testing. Additional reports comparing treatment options will greatly benefit the medical care for this condition.







