POST-TREATMENT MRI frequently underestimates tumor size in patients with invasive lobular carcinoma (ILC) who receive neoadjuvant therapy, according to new findings that may influence surgical planning in this breast cancer subtype.
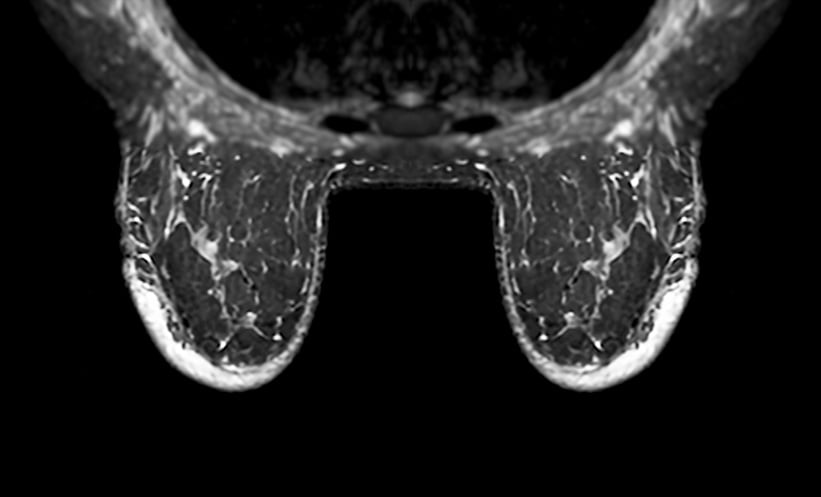
ILC represents 10–15% of breast cancer cases and is known for a diffuse growth pattern that makes it difficult to assess using conventional imaging. While breast MRI is typically used to evaluate ILC, its accuracy after neoadjuvant chemotherapy (NAC) or endocrine therapy (NET) has been unclear. This retrospective study examined MRI reliability and its impact on surgical margins.
Researchers analyzed 129 patients with ILC who underwent NAC or NET followed by post-treatment MRI. They defined a discrepancy as a 0.5 cm or greater difference between the MRI-reported longest tumor diameter and the pathological measurement. The team also assessed tumor imaging phenotypes: mass, non-mass enhancement (NME), or a combination.
Findings revealed that MRI underestimated tumor size in more than half of the cases (52.5%), matched pathology in 25.3%, and overestimated size in 22.2%. Underestimation was especially pronounced in tumors with NME, where 62.5% of cases showed significant underreporting compared to 39.5% in mass-only lesions. The average underestimation in NME cases was 3.4 cm.
This imaging inaccuracy had direct surgical implications. Patients whose tumor size was underestimated were more likely to have positive surgical margins following breast-conserving procedures (p = 0.018). Furthermore, in patients who showed a complete imaging response on MRI, 93.3% still had residual invasive disease upon pathological examination.
These results underscore the limitations of MRI in the surgical planning of ILC after neoadjuvant therapy. Surgeons should account for the potential underestimation of tumor size, particularly in cases involving NME, to optimize resection strategies and reduce the likelihood of incomplete tumor removal.
Reference:
Vertido A et al. Accuracy of Breast MRI for Surgical Planning After Neoadjuvant Therapy for Patients with Invasive Lobular Carcinoma. Ann Surg Oncol. 2025. doi:10.1245/s10434-025-17735-6. [Online ahead of print]