BACKGROUND AND AIMS
The association between cholesterol and cardiovascular disease (CVD) risk is attenuated in patients with rheumatoid arthritis (RA).1 In fact, patients with RA in the lowest low-density lipoprotein (LDL) group (<70 mg/dL) may experience an unexpectedly high CVD risk.2 The authors explored whether patients with LDL <70 mg/dL (Group 1) had higher coronary atherosclerosis burden compared to other LDL groups (Group 2: 70≤LDL≤130 mg/dL; Group 3: LDL>130 mg/dL), as a reason for this risk. The authors further evaluated whether low LDL in Group 1 associated with differences in inflammation, LDL particle composition, or oxidation.
MATERIALS AND METHODS
One hundred and fifty patients with no history of CVD, from the previously described PROTECT-RA cohort,3 underwent coronary atherosclerosis evaluation with CT angiography. Coronary artery calcium, number of segments with plaque (segment involvement score), stenotic severity (segment stenosis score), and extensive (>4 segments with plaque) or obstructive disease (>50% stenosis) were assessed. Lipoprotein classes and subclasses were directly measured using single vertical spin density gradient ultracentrifugation. Oxidised LDL (oxLDL) was measured with monoclonal antibody E06. Chemiluminescence ELISA quantified IgG and IgM antibodies to oxLDL (anti-oxLDL) and apolipoprotein (apo)B100 immune complexes (IC). Pro-inflammatory cytokines were measured with Erenna® Immunoassay (Singulex, Alameda, California, USA). Robust linear and logistic regression models evaluated associations between LDL groups and plaque outcomes; both models were adjusted for Framingham modified cardiovascular risk score, obesity, disease activity, biological disease-modifying anti-rheumatic drugs, and statin treatment. Similar models evaluated adjusted differences in LDL subclasses, oxLDL, anti-oxLDL, anti-apoB100 IC, and cytokines across LDL groups.
RESULTS
Patients were predominantly female with seropositive, erosive, and well-controlled disease. Group 1 patients had higher coronary plaque burden (Figure 1A) and 2.8-times greater risk of extensive or obstructive disease (adjusted odds ratio: 2.82; 95% confidence interval [CI]: 1.12–7.17; p=0.031) compared to LDL >70 groups. No differences in RA-related inflammation were observed across LDL groups that could explain disparity in LDL levels. However, statin-naïve patients with LDL <70 mg/dL exhibited greater oxLDL (log-transformed estimated marginal means [EMM]: 2.55, 95% CI: 2.34–2.77; versus 2.27, 95% CI: 2.19–2.36, p=0.018 for LDL >70). Moreover, Group 1 patients exhibited greater serum levels of IgG anti-oxLDL and apoB100 IC than higher-LDL groups (Figure 1B). This was not the case for their IgM counterparts. LDL subclass-relative content in the LDL particles differed across groups (Figure 1C). Lipoprotein (a) (Lp[a]) was higher in LDL particles in Group 1 (EMM: 16.04%, 95% CI: 11.75–20.33; versus 10.48%, 95% CI: 8.20–12.75, p=0.026 in Group 2; and 7.41%, 95% CI: 0.77–14.04, p=0.033 in Group 3). Notably, Lp(a) content strongly associated with oxLDL overall (r=0.83; p<0.0001); this association was stronger for Group 1 compared to others (p<0.005; Figure 1D). Immune recognition of oxLDL, specifically IgG anti-oxLDL and anti-apoB100 IC, associated with higher TNFα and IL-6 elaboration. IL-6 was higher in Group 1 (log-transformed EMM: 1.98, 95% CI: 1.64–2.32; versus 1.57, 95% CI: 1.45–1.70, p=0.028 in Group 2; and 1.32, 95% CI: 0.84–1.80, p=0.031 in Group 3). IL-6 associated with both IgG anti-oxLDL (p=0.015) and anti-apoB100 IC (p=0.016). IL-6 further associated with higher coronary artery calcium (adjusted B [association between IL-6 and coronary artery calcium]: 0.41; 95% CI: 0.01–0.81; p=0.049).
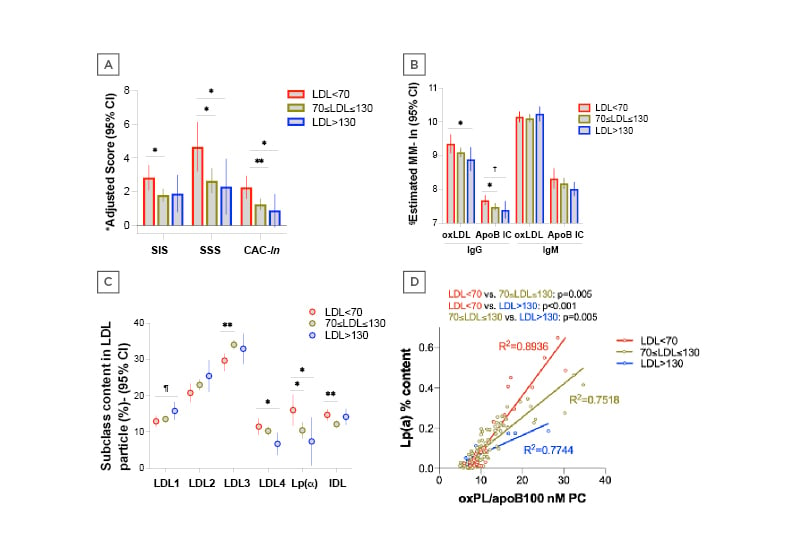
Figure 1: Coronary plaque burden, lipoprotein particle structure and oxidation differences across LDL strata in RA. A) Patients with LDL <70 mg/dL had higher coronary plaque burden compared to higher LDL groups. Model adjusted for Framingham D’Agostino risk score, obesity, DAS28-CRP, bDMARD use, and statin use. B) Patients with the lowest LDL exhibited greater serum levels of IgG anti-oxLDL and apoB100 IC than higher LDL groups. This was not the case for IgM anti-oxLDL and apoB100 IC. Model adjusted for Framingham D’Agostino risk score and statin use. C) LDL particle composition differs across various LDL groups. Model adjusted for Framingham D’Agostino risk score, statin use, and total HDL. D) The association between Lp(a) content and LDL oxidation appears stronger in patients with LDL <70 mg/dL compared to higher LDL groups. Models adjusted for Framingham D’Agostino risk score and statin use.
ApoB100 IC: apolipoprotein B100 immune comeplexes; bDMARD; biologic disease-modifying anti-rheumatic drugs; CAC-ln: log-transformed coronary artery calcium score; CI: confidence interval; DAS28-CRP: disease activity score-28 for rheumatoid arthritis with C-reactive protein; EMM: estimated marginal means; HDL: high-density lipoprotein; LDL: low-density lipoprotein; Lp(a): lipoprotein (a); nMPC: nonlinear model predictive control; oxLDL: oxidised LDL; oxPL: oxidised phospholipids; RA: rheumatoid arthritis; SIS: segment involvement score; SSS: segment stenosis score, p=0.056, † p=0.051, *p<0.05, **p<0.01
CONCLUSION
Patients with RA with LDL <70 mg/dL had higher coronary atherosclerosis burden. Low circulating LDL in that group may reflect higher oxidation; this was mostly linked to the larger Lp(a)-relative content of LDL and the significantly higher oxidation potential in that group. Greater LDL oxidation and immune recognition of oxLDL further associated with higher IL-6 elaboration, which may in turn augment atherosclerosis burden in the low-LDL group.