INTRODUCTION AND OBJECTIVES
Urolithiasis may cause urinary tract infections, infections can cause urolith formation, and surgery for urolithiasis carries risk of infectious complications.1,2 The European Association of Urology (EAU) guidelines recommend peri-operative antibiotic prophylaxis for stone removal, but do not specify the type or duration.3 The authors studied the results of stone cultures in percutaneous nephrolithotomy (PCNL), and its relationship to preoperative urine testing and postoperative systemic inflammatory response syndrome (SIRS).
MATERIALS AND METHODS
A total of 424 consecutive PCNL procedures performed in two medical centres during the period of January 2018–September 2023 were included. Urine was directly sent for culture in at-risk patients or if a urine test strip showed the presence of leucocytes or nitrite. During PCNL, stone fragments were collected on sterile gauze and placed in a container that was sent to the microbiology laboratory. Following this, the entire specimen was inoculated in a brain heart infusion agar of thioglycolate broth, and then assessed after 5–7 days for signs of growth. If present, subculture was performed onto blood agar plates. These plates were incubated aerobically and anaerobically to identifythe microorganism.
RESULTS
Stone cultures were obtained in 338 (80%) surgeries, with 145 (46%) being positive. Preoperative urine testing was performed before 391 (92%) procedures, of which 143 (41%) were positive. Enterococcus faecalis was the most commonly cultured microorganism on stones (n=28, 19%) and Escherichia coli was the most commonly cultured microorganism in urine (n=49, 34%; Figure 1). Of all patients with clean preoperative urine, 26% had a positive stone culture. Of patients with a positive preoperative urine culture, 47% had the same microorganism in the stone culture, 21% had a different microorganism, and 32% had a negative stone culture. Positive stone cultures were significantly associated with an increased risk of postoperative SIRS (odds ratio: 3.3; 95% CI: 1.3–8.2), while urine cultures were not (odds ratio: 1.7; 95% CI: 0.76–3.6).
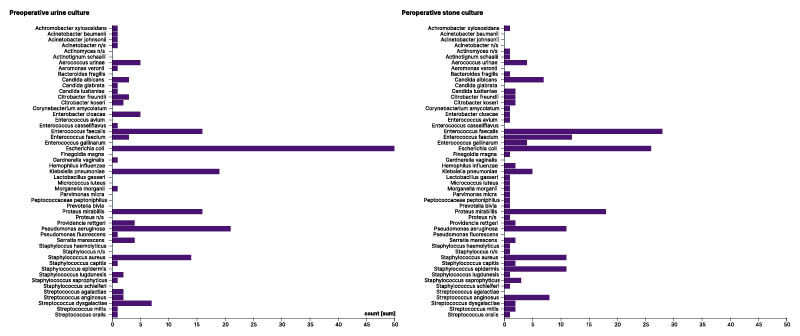
Figure 1: Results of the preoperative urine cultures and perioperative stone cultures.
CONCLUSION
Stone cultures are often positive, are poorly predicted by preoperative urine cultures, and are associated with an increased risk of postoperative SIRS. Intraoperative stone cultures provide additional information regarding the colonised status of the urinary tract.







