Abstract
Massive haemoptysis, which can result in abrupt respiratory failure, is a potentially fatal consequence of pulmonary tuberculosis. Radiologically, it can present as a complete collapse of one lung due to endobronchial clot formation. Here, the authors report two cases, one of whom was a female who was pregnant and near term, who presented with massive haemoptysis followed by severe respiratory distress. Fibre optic bronchoscopy was performed in both cases, and clots were retrieved. One of the patients required intubation and invasive mechanical ventilation. The procedure was technically difficult because of the acute hypoxaemia, necessitating a team of pulmonologists and anaesthetists. Bronchoalveolar lavage enabled the authors to clinch the diagnosis. Post-procedure, both patients showed rapid clinical and radiological improvement. In resource-limited settings where rigid bronchoscopy is not available, fibre optic bronchoscopy can be performed for clot retrieval, as it can be a life-saving procedure for the patient.
Key Points
1. Massive haemoptysis with unilateral complete lung collapse and rapid respiratory failure are life-threatening complications of pulmonary tuberculosis. In order to clear the airways, this necessitates immediate hospitalisation and blood clot extraction.
2. Fibre optic bronchoscopy with saline lavage and forceps extraction can be used to enable clot removal in a piecemeal manner in resource-constrained areas when rigid bronchoscopy facilities are not accessible.
3. A suction catheter can be inserted over a paediatric fibre optic bronchoscope and progressed to the location of the obstruction. After this, bronchoscope should be removed and a direct connection made between the suction catheter and suction port. This enables removal of a large blood clot.
INTRODUCTION
Any haemoptysis exceeding 100 mL/hr, causing abnormal gas exchange/airway obstruction or leading to haemodynamic instability is defined as life-threatening or massive haemoptysis.1 Few case reports have described blood clot formation secondary to massive haemoptysis leading to airway obstruction.2 Here, the authors report two cases who presented within a span of 1 month, where massive haemoptysis lead to acute respiratory failure. On radiology, there was unilateral complete lung collapse. Flexible bronchoscopy was used in both instances to remove the clots. Pulmonary tuberculosis (PTB) was the underlying aetiology in both cases.
CASE REPORT 1
A 19-year-old female presented to the emergency room with complaints of dyspnoea, cough with expectoration for 1 week, and chest pain for 2 days. They had a history of massive haemoptysis 7 days before. Blood was bright red, measuring approximately 300–400 mL. The patient received numerous injections from a local doctor in order to achieve haemostasis. They had no history of any other skin or mucosal bleed, and no comorbidities. There was no history of prior antitubercular treatment or contact with patients with tuberculosis. On examination, they were dyspnoeic maintaining a saturation of peripheral O2 (SpO2) of 95% with a non-rebreathing face mask at 15 L/min, respiratory rate of 28 /min, pulse rate of 124 /min, and blood pressure (BP) of 108/62 mmHg. PaO2/FiO2 ratio was 76 (FiO2 approximately 100%). Chest X-ray showed opaque haemithorax with an ipsilateral mediastinal shift (Figure 1A). On high-resolution CT (HRCT) there was collapsed left lung with an abrupt cut-off of the left mainstem bronchus (Figure 1B).
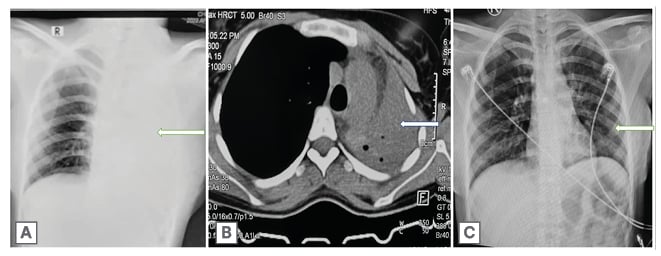
Figure 1: Radiological findings in case 1.
1A) Chest X-ray showing opaque hemithorax with ipsilateral mediastinal shift (white arrow).
1B) HRCT showing collapse of left lung with abrupt cut off of left mainstem bronchus (white arrow).
1C) Chest X-ray post procedure showing resolution of lung collapse (white arrow).
HRCT: high-resolution CT.
The patient was admitted to the intensive care unit in an isolated cubicle and kept on a high flow nasal cannula at 60 L/min. A fluid bolus of 800 mL (20 mL/kg) was given over 30 minutes. Mean BP was below 65 mmHg; thus, dopamine (the first line inotrope of choice in the author’s institution for when central venous access is not available) infusion was started at 5 µg/kg/min to prevent hypovolemic shock and renal hypoperfusion. A quick bedside check video bronchoscopy revealed blood clots obstructing the entire left mainstem bronchus. The procedure was abandoned due to significant desaturation. Haemoglobin was 13.2 g/dL. No blood transfusion was required. Total leukocyte count, platelet count, and liver and kidney function tests were within normal limit. The next day, the patient was shifted to the operating theatre and electively intubated. Due to non-availability of rigid bronchoscopy, which is the ideal procedure here, a video bronchoscopy was done via an endotracheal tube of size 8 mm. Clots were retrieved with biopsy forceps of size 2.4 mm and foreign body forceps. However, a few large clots could not be extracted with forceps or suctioned via bronchoscope working channel. Hence, the authors employed a paediatric fibre optic scope over which a flexible 18 French suction catheter was positioned. The left mainstem bronchus was reached with the bronchoscope and suction catheter, which were then removed, leaving the catheter in place and being advanced further. The catheter was connected to the suction channel and a large blood clot was removed. Remaining clots were suctioned subsequently and patency was achieved in all the lobes. Bronchoalveolar lavage (BAL) was collected for further testing. The patient was extubated on the table and kept on facemask at 4 L/min. There was resolution of lung collapse on chest X-ray (Figure 1C). The next day, the patient had a SpO2 of 97% on room air and a BP of 120/72 mmHg.
Mycobacterium tuberculosis was detected on BAL GeneXpert (Cepheid, Synnyvale, California, USA). The patient was initiated on anti-tubercular treatment (ATT) based on their weight band, and is under follow-up.
CASE REPORT 2
A 21-year-old female, 37 weeks pregnant, presented to the emergency room with complaints of dyspnoea, cough, and chest pain for the past 6 days. They had a history of massive haemoptysis 6 days prior. Due to concerns about haemoptysis reoccurring, their scheduled normal vaginal delivery was cancelled, and they instead had a lower segment Caesarean section under spinal anaesthesia at a private hospital. The haemoptysis was bright red and approximately 500 mL. There was no history of fever, loss of appetite, or weight loss, and no comorbidities or prior respiratory illness. Post-lower segment Caesarean section, the patient became symptomatic and hypoxic. They were managed with O2 and other supportive care at a private hospital. The neonate was healthy. At presentation, the patient was severely dyspnoeic with a SpO2 of 60% at room air and 92–98% with non-rebreathing face mask at 15 L/min. They had tachycardia, tachypnoea, and their BP was 100/70 mmHg. They were admitted to the intensive care unit in an isolated cubicle. Chest X-ray showed opaque right hemithorax (Figure 2A). On HRCT there was collapse consolidation of right lung parenchyma with ipsilateral mediastinal shift and minimal right-sided pleural effusion. (Figure 2B). A short bedside check fibre optic bronchoscopy revealed complete occlusion of the right mainstem bronchus by blood clots. The patient was shifted to the bronchoscopy suite, and video bronchoscopy was performed under minimal sedation with 1 mg of intravenous midazolam without intubation and invasive mechanical ventilation. Blood clots were removed with saline lavage, biopsy forceps of size 2.4 mm, and foreign body forceps. The procedure took approximately 2 hours, and patency of the entire right lung airways was achieved. Patient saturation improved gradually during the procedure. BAL was taken from the right lower lobe. Within the next 24 hours, all vitals were stable. Chest X-ray showed marked radiological clearing (Figure 2C). BAL for acid-fast bacilli was 1+ and GeneXpert detected mycobacterium tuberculosis (TB), which was rifampicin sensitive. Bacterial and fungal cultures were sterile. ATT was started in accordance with the patient’s weight band, and the patient is under follow-up.
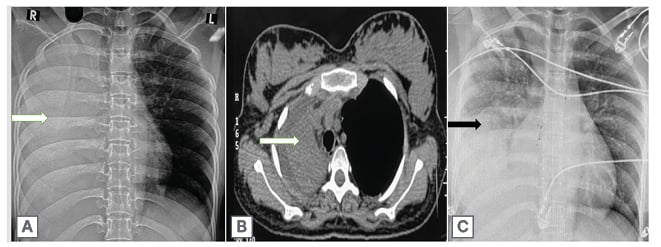
Figure 2: Radiological findings in case 2.
2A) Chest X-ray showing complete collapse consolidation of right lung (white arrow).
2B) HRCT showing complete collapse consolidation of right lung parenchyma with ipsilateral mediastinal shift and minimal right sided pleural effusion (white arrow).
2C) Chest X-ray showing significant radiological improvement post procedure (black arrow).
HRCT: high-resolution CT.
DISCUSSION
India is a country with a high burden of TB. The World Health Organization (WHO) TB statistics for India for 2021 give an estimated incidence figure of 2.59 million cases, 188 cases per 100,000 population.3 A cough lasting for more than 2 weeks, chest pain, haemoptysis, weakness or fatigue, weight loss, lack of appetite, chills, fever, and night sweats are the common symptoms associated with PTB. Sputum microscopy, culture test, as well as the newer molecular tests such as GeneXpert and Truenat are helpful in diagnosis.3 TB was found in 79.2% of patients with haemoptysis, according to an Indian study.4 The majority of patients with a diagnosis of TB have a good outcome. This is mainly because of effective treatment. Without treatment mortality rate for tuberculosis is more than 50%.5 According to the Global TB report, response to ATT was 85% among new and relapsed cases of PTB in India, when treated with the standard four drug regimen.6
Several disorders have been described where an endobronchial blood clot can lead to airway obstruction. A few benign conditions include PTB, bronchiectasis, vasculitis, invasive fungal infections, bleeding disorders, post-tracheotomy, and trauma during suctioning. Malignant diseases include bronchogenic carcinoma, carcinoid tumours, metastatic pulmonary nodules, and other similar diseases. A history of mild or massive haemoptysis may be found before an endobronchial blood clot formation in most cases; however, respiratory failure is seen in approximately 30% of patients without a previous history of haemoptysis.2
PTB presenting as massive haemoptysis followed by clot formation could be a life-threatening complication, as it can lead to respiratory failure. Active PTB is a hypercoagulable state as these patients show low haemoglobin, elevated total leukocyte count, platelet count, plasma fibrinogen, factor VIII, plasminogen activator inhibitor 1, and decreased antithrombin III and protein C levels. Etamsylate is commonly administered to control bleeding. It works by increasing capillary vascular resistance and platelet adhesiveness.7 In pregnancy there is an elevation of factors VII, VIII, and X, as well as fibrinogen, and von Willebrand factor, leading to a marked increase in procoagulant activity, which is maximal around the term. Prothrombin fragments and thrombin–antithrombin complexes are increased. Protein S activity is significantly reduced along with activated protein C resistance. As a result, overall fibrinolytic activity is impaired during pregnancy.8,9 Bleeding in the authors’ case could be the result of one or more of the above factors. Table 1 gives the description of the two cases in which PTB in pregnancy caused severe haemoptysis and the development of endobronchial clots that resulted in total lung collapse, which to the best of the authors’ knowledge are the only two cases published in literature.
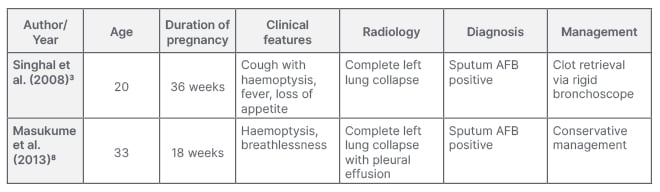
Table 1: Case reports of complete lung collapse in pregnancy with pulmonary tuberculosis as the underlying aetiology.
AFB: acid-fast bacilli.
Initial management of endobronchial clot includes evaluation by fibre optic bronchoscopy, followed by saline lavage and suctioning. If unsuccessful, this is followed by extraction with the help of biopsy forceps, either en bloc or in piecemeal fashion. Rigid bronchoscopy is the preferred technique for suctioning and forceps extraction of blood clots. It enables effective tamponade of the bleeding airway preventing the contralateral lung from getting affected. Recently, techniques for the dissolution of blood clots with the help of topical thrombolytics, such as streptokinase, urokinase, and tissue plasminogen activator have also been described.7,10,11 Cryotherapy via flexible bronchoscopy can also be used for clot removal.12,13
CONCLUSION
Massive haemoptysis secondary to pulmonary tuberculosis can lead to complete lung collapse and acute respiratory failure. Use of fibre optic bronchoscopy for clot removal is a time-consuming process, as they have to be removed in piecemeal fashion. However, this can be a life-saving procedure for patients in centres where advanced bronchoscopic techniques like cryoextraction and rigid bronchoscopy are not available.







