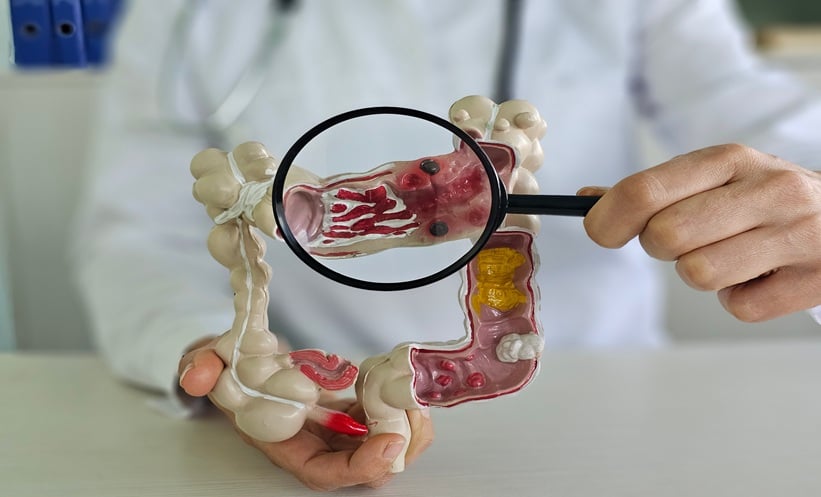
PSYCHIATRIC disorders were associated with a markedly increased risk of colorectal cancer in a large UK population study, highlighting an overlooked cancer risk in people with mental health conditions.
A new matched cohort analysis using data from the UK Biobank showed that individuals with clinically diagnosed psychiatric disorders experienced almost double the risk of developing colorectal cancer compared with those without psychiatric diagnoses. The findings emphasised the importance of integrating cancer prevention strategies into mental healthcare.
Psychiatric Disorders and Colorectal Cancer Risk
Colorectal cancer is among the most frequently diagnosed cancers globally and remains a leading cause of cancer-related mortality. Early identification of high-risk populations is therefore essential. Although psychiatric disorders have previously been associated with several malignancies, evidence linking them specifically to colorectal cancer has been limited.
To address this gap, researchers examined data from 29,769 adults with new-onset psychiatric disorders recorded after enrolment into the UK Biobank. Individuals with a previous cancer diagnosis, apart from non-melanoma skin cancer, were excluded. Each psychiatric disorder case was matched with individuals without psychiatric diagnoses to minimise confounding.
During a median follow-up of 5.69 years, 190 colorectal cancer cases were identified among individuals with psychiatric disorders, corresponding to an incidence rate of 1.13 per 1,000 person-years. In comparison, 921 cases occurred in the reference group, with an incidence rate of 0.53 per 1,000 person-years. Statistical analysis using Cox proportional hazards models demonstrated a significantly increased hazard of colorectal cancer associated with psychiatric disorders (hazard ratio: 1.93; 95% CI: 1.64–2.27).
Greater Risk Seen with Multiple Psychiatric Disorders
The study also showed an increased risk of colorectal cancer in individuals diagnosed with multiple psychiatric disorders. Participants with more than one psychiatric condition had a higher hazard of colorectal cancer than those with a single diagnosis (hazard ratio: 2.53; 95% CI: 1.90–3.37 versus 1.78; 95% CI: 1.48–2.13; p<0.05).
Several mechanisms may underlie this association, including lifestyle factors such as smoking, diet, and physical inactivity, as well as reduced engagement with colorectal cancer screening programmes. Biological pathways related to chronic psychological stress, inflammation, and immune dysregulation may also contribute. However, as an observational study, the findings could not establish causality.
The authors emphasised the need for enhanced monitoring, early intervention, and equitable access to cancer screening for patients with psychiatric disorders. These results support a more integrated approach to mental and physical healthcare, with potential implications for colorectal cancer prevention strategies.
Reference
Wang Z et al. Psychiatric disorders associated with increased risk of colorectal cancer in the UK biobank cohort. Sci Rep. 2026: DOI;10.1038/s41598-025-31083-1.