HEPATITIS-ASSOCIATED aplastic anaemia can be successfully treated with early haematopoietic stem cell transplantation after liver transplantation, with excellent survival and long-term outcomes reported in a small but extremely high-risk paediatric cohort. New findings highlight the potential of timely transplantation strategies in a condition that is rare, rapidly progressive, and often life threatening.
Hepatitis-Associated Aplastic Anaemia
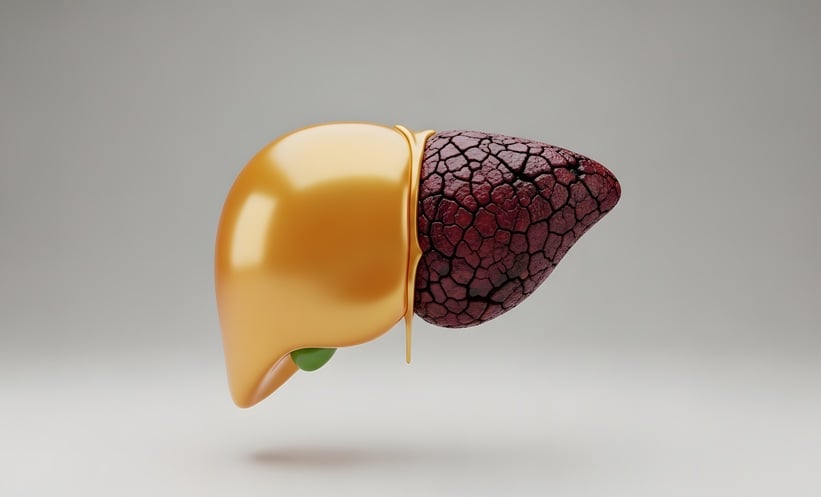
Hepatitis-associated aplastic anaemia is an uncommon disorder that can progress rapidly to liver failure, requiring urgent liver transplantation. Management becomes particularly complex when severe aplastic anaemia develops following transplantation, as patients are clinically fragile and highly vulnerable to complications. Although immunosuppressive therapy has shown some benefit in selected cases, its delayed onset of action and limited suitability in critically ill patients restrict its wider use. Haematopoietic stem cell transplantation using matched related donors has previously been described as curative, but outcomes with alternate donors have been less consistent.
Paediatric Experience with Early Transplantation
Investigators reported outcomes in 10 children with hepatitis-associated aplastic anaemia who underwent haematopoietic stem cell transplantation following liver transplantation. This cohort represented an exceptionally high-risk group, with most patients receiving stem cells from alternate donors rather than matched related donors. Despite these challenges, overall survival was 90% at a median follow up of 38 months after liver transplantation.
All surviving children achieved normal blood counts and normal liver function, with good performance status at last follow up. Importantly, no liver related complications were observed after stem cell transplantation, and no cases of significant graft versus host disease were reported. These findings suggest that concerns regarding transplant related toxicity and immune complications may be mitigated with careful patient selection and close monitoring.
Managing Complications Through Multidisciplinary Care
Multiple infectives and non-infective complications occurred following stem cell transplantation, reflecting the complexity of care in this population. However, all complications were successfully managed through coordinated multidisciplinary input involving liver transplantation specialists, haematology teams, and intensive supportive care services.
Reference
Meena SK et al. Excellent outcomes in children after haematopoietic stem cell transplantation for hepatitis-associated aplastic anaemia following liver transplantation. BJ Haem. 2026;https://doi.org/10.1111/bjh.70328.