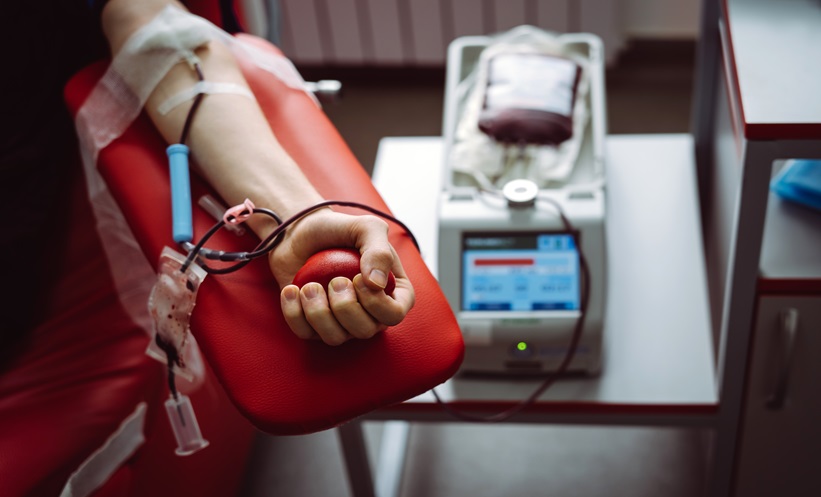
PLATELET transfusion practices in neonates and children show substantial variation, with donor and platelet processing characteristics strongly associated with posttransfusion platelet increments and overall transfusion burden but not with adverse clinical outcomes.
Epidemiology of Platelet Transfusion in Children
Platelet transfusion is a critical intervention for patients at risk of bleeding, particularly in neonatal and paediatric settings. In a large multicentre cohort study analysing 249 340 inpatient encounters, platelet transfusion was administered to 3.6% of patients younger than 18 years of age. Transfusion rates varied by age, occurring least frequently in children younger than 1 year and most commonly in those aged 1 to less than 6 years. Neonates received higher weight-based platelet doses than older children, and median pretransfusion platelet counts were significantly higher in neonates than in older paediatric patients. After excluding patients with bleeding, most platelet transfusions in both groups occurred at relatively high pretransfusion platelet thresholds, highlighting considerable heterogeneity in clinical practice.
Platelet Transfusion and Donor Characteristics
Several platelet processing and donor factors were independently associated with lower posttransfusion platelet increments. Use of platelet additive solution, pathogen reduction, and platelet storage durations longer than 3 days were all linked to reduced platelet count responses. Donor related factors also influenced increments, with lower responses observed for platelets from male donors and from donors aged 40 years or older. These associations were consistent across analyses and remained significant after adjustment, suggesting that both product processing and donor characteristics meaningfully affect the immediate effectiveness of platelet transfusion in paediatric recipients.
Transfusion Burden and Clinical Outcomes
In addition to reduced platelet increments, the same platelet transfusion and donor factors were associated with a higher overall transfusion burden. Use of platelet additive solution, pathogen reduction, longer storage duration, and older donor age increased the likelihood of patients requiring subsequent platelet transfusions. However, despite these differences in transfusion burden, no associations were observed between these factors and hospital length of stay or mortality. This finding suggests that while certain platelet characteristics may influence transfusion efficiency, they do not appear to translate into worse short term clinical outcomes. The results provide a comprehensive overview of platelet transfusion practices in neonates and children and underscore the need for prospective studies to inform optimisation of platelet selection and transfusion strategies in paediatric care.
Reference
Goel R et al. Platelet transfusion practices and outcomes in neonates and children. JAMA Netw Open. 2026;9(1):e2554531.