Abstract
Objective: The COVID-19 pandemic is still showing fluctuating trends and rapidly increasing case numbers, naturally creating a significant air of panic and hopelessness. This study aimed to investigate the mental health status of doctors in comparison to non-doctors, and its suggestive determinants amidst the COVID-19 pandemic.
Methods: An online cross-sectional survey was conducted during January–March 2021, using a convenience sampling technique. A sample size of 377 was calculated through RaoSoft (RaoSoft Inc., Seattle, Washington, USA) software. Inventories used are Zung Self-Assessment Anxiety Score (SAS) and Self-Assessment Depression Score (SDS), for the purpose of comparing different groups. The survey was distributed as an online Google form via social media. Results were evaluated by IBM Statistical Package for Social Sciences version 26.0 (Endicott, New York, USA).
Results: A total of 395 participants responded, out of which 10% showed extreme levels of anxiety. Among doctors, 14% had moderate levels of anxiety while 10% of unmarried respondents had extreme self-reported anxiety. Out of non-doctors, 15% showed signs of depression, among which a moderate level of depression was seen in 13% males, and severe depression was seen in 4% of married respondents. Higher depression scores were recorded in non-doctors, while there was no significant difference in anxiety levels of both groups.
Conclusion: A significant impact on mental health has been noted in various groups of respondents, with severe depression as well as severe anxiety. This should be alarming enough to instigate authorities to conduct mental health programs to counter this negative impact of COVID-19. Quick interventions and strategies can save countries from a grim future.
INTRODUCTION
The first case of the novel COVID-19 in Pakistan was reported on 26th February 2020 in its trade-hub city, Karachi. Pakistan entered its first lockdown in March 2020. Educational institutes, markets, trade centres, and entertainment centres were closed. Though the lockdown lasted for just a few weeks, it was enough to trigger mass panic, fear, and depression. Since then, more than 900,000 people have been affected and 20,465 deaths have been reported to date by the Ministry of National Health Services Pakistan.1 According to National Health Services, Regulations, and Coordination (NHSRC), doctors are the most affected segment of healthcare providers as 3,275 (61%) have so far contracted the viral infection, followed by 1,453 paramedics. A total of 27% healthcare providers have been infected with the virus.2
Globally, healthcare workers have been frequent victims of COVID-19 and face the stigma of being carriers. A study reported a high percentage of individuals who believed that social interactions with healthcare workers during pandemics should be avoided.3 In earlier reports, the incidence of COVID-19 was recorded to be about 29% in healthcare individuals.4 Their moral obligation towards duty and social isolation leaves them in a dilemma, which is yet again a challenge for mental health.
It is very well known that the initial phase of virus spread was associated with high levels of unfamiliarity and uncontrollability, which made it difficult for healthcare workers to adopt a safe and effective action plan.5 In addition, fake news and myths regarding this virus were widespread on social media, making it even more difficult for doctors and authorities to function properly. There are sour memories of past pandemics, where high mortality rates and infection in healthcare providers were recorded. A study in Canada recorded that around 37% of total cases of severe acute respiratory syndrome were in healthcare providers.6 Keeping in view all of these circumstances, anxiety and depression among doctors is not unexpected. Studies are predicting a high impact on mental health as a result of this pandemic.4 The unpredictable nature of the course of the disease, unexpected post-infection consequences, new emerging mutated forms of the virus, and rumours of fourth and fifth hybrid waves in Pakistan could nevertheless increase psychological strain on healthcare workers.
Moreover, there is a lack of availability of essential resources such as medications, isolation wards, personal protective equipment,7 oxygen cylinders, and artificial ventilation systems across Pakistan, which has compromised the standard of healthcare provided to the public.8 Acknowledging the need and still not being able to provide optimum services due to limitations has challenged communities, and added to the psychological strain on frontline workers, including doctors, nurses, and paramedics. This has left many healthcare workers in a dilemma, questioning their moral stance.8
Despite providing mass vaccination, the healthcare burden has undoubtedly been one of the major concerns of every country. The COVID-19 crisis has targeted the economical sustainability of many countries, especially developing countries like Pakistan and Bangladesh. The Asian Development Bank predicted the Pakistani economy would decrease by 3.3% in 2019 to 2.6% by 2020, and inflation was likely to persist around 11.5% for 2020.9 With the addition of a health emergency in the country, it is not difficult to imagine the economic blow that Pakistan is facing. Economic recession, unemployment, and fear of food unavailability has inevitably flared up the rising trends of stress, anxiety,10 and suicide rates in society.11,12
Recent studies have reported 20–44% of adults with clinical levels of anxiety and depression.13 It is well established that depression is a leading cause of 90% of global suicide cases.14 The first suicide case due to the COVID-19 pandemic was reported from Bangladesh.15 In Japan, around a 70% rise in female suicide cases was observed after COVID-19.16 Sixteen suicide cases have been reported in Pakistan during COVID-19. The reason behind most of the suicide cases was the fear of being infected by the virus.17 The rapidly increasing counts of COVID-19 victims that individuals see every day on social networks have naturally created a significant air of panic and hopelessness. Studies conducted during the H1N1 and severe acute respiratory syndrome pandemics show that pandemics and lockdowns have always put a strain on mental health issues. Social isolation has been marked as one of the major causes of depression in such scenarios.4
The good mental health of an individual is valuable and allows them to provide optimum services to society. As this pandemic is projected to last for a long time, more research is needed to evaluate mental health status in Pakistan. This study aimed to investigate the mental health status of doctors in comparison to non-doctors, its suggestive determinants amidst the COVID-19 pandemic, and to determine which category among the public is most psychologically affected by this outbreak. These results can regulate appropriate intervention and modifications, and aid medical workers and the public alike.
METHODOLOGY
An online cross-sectional survey was conducted from January–March 2021 among doctors and non-doctors of four major cities in Pakistan: Karachi, Lahore, Rawalpindi/Islamabad, and Peshawar. The participants were recruited online using the convenience sampling technique. In the study, doctors are defined as all those who have a Bachelor’s degree in medicine and surgery or medical doctors, while non-doctors are individuals from all other professions with a minimum qualification of 10 years of schooling. Several steps were taken to ensure data quality. Firstly, participants were asked personal details in demographics regarding profession and level of education. Those who provided nonsensical responses were removed from the analysis. All who were below 20 years of age or lacked minimum qualifications were not included in the study. Based on the target population, the margin of error was 5.0%, and confidence interval 95%. The sample size calculated through RaoSoft software (RaoSoft Inc., Seattle, Washington, USA) was 377. A total of 406 participants began the questionnaire. Out of these, three were rejected because they were less than 20 years of age and five were excluded because of incomplete responses. Three questionnaires with nonsensical responses were also excluded from the analysis. After rejecting 11 questionnaires, 395 questionnaires were used for result analysis.
Participants were invited to fill in an online questionnaire designed using Google (Mountain View, California, USA) forms via WhatsApp (Meta Platforms, Cambridge, Massachusetts, USA), Facebook (Meta Platforms), and email. The nature and purpose of the survey were explained in the message preceding the link to the survey. All participants were encouraged to forward the link to acquaintances, thereby approaching a larger number of respondents.
For psychological distress evaluation, the internationally recognized Zung Self-Rating Anxiety Scale (SAS)18 and Zung Self-Rating Depression Scale (SDS)19 were used. Ethical permission was not required. A set of 30 questions was asked in total, where each question carried a different score depending on the response.20
In the anxiety assessment, 10 questions were asked and the participant had to choose one response from: ‘Never’, ‘Sometimes’, ‘Half the time’, ‘Frequently’, and ‘Always’. Each response had a score from 0 to 4, which was totalled at the end of the survey. The total score was then calculated out of 40 points. The participants whose total score lay between 0–8 points had minimal anxiety; 8–16 points had mild anxiety; 17–24 points had moderate anxiety; and 25 points and above showed high and extreme anxiety.
For the depression assessment, a total of 20 questions were asked, and the participant had to choose from: ‘Never’, ‘Sometimes’, ‘Good part of the time’, and ‘Mostly’. These responses were scored from 1 to 4 and the total score was calculated out of 80 points. Participants with less than 50 points had no depression and were marked ‘normal’. Those with 50–59 points had mild depression, while those with 60–69 points had moderate depression. Severe depression was diagnosed for all those with 70 points or more. Responses were downloaded from the online survey and processed as a spreadsheet.
Frequency tables and proportions were computed to summarise the data. Data were stratified into different groups based on demographic characteristics and the anxiety and depression levels of the participants to give an in-depth insight into the descriptive statistics of the study. Since the data did not conform to a normal distribution, the Mann–Whitney U test for Independent Samples was used to compare SAS and SDS scores between the two different groups. One-way Analysis of Variance test with post hoc Bonferroni correction was applied when the variable consisted of more than two groups. All analysis was performed using IBM Statistical Package for Social Sciences version 26.0 (Endicott, New York, USA). A p<0.05 was taken as significant.
RESULTS
Participants’ demographic profile has been summarised in Table 1. In total, 395 participants completed the survey. Among them, 260 (65.8%) were female and 214 (54.1%) were married. There were 212 (53.6%) participants belonging to the age group of 20–30 years. Most of the respondents held a Master’s degree or above (179; 45.3%). Respondents belonged to different provinces of Pakistan, with 204 (51.6%) residing in the twin cities, Islamabad and Rawalpindi. Over half of participants (51.6%; 306) reported that they had not suffered from COVID-19, while 6 (1.5%) were suffering at the time of filling the survey form and 83 (21.0%) of participants had recovered from infection.
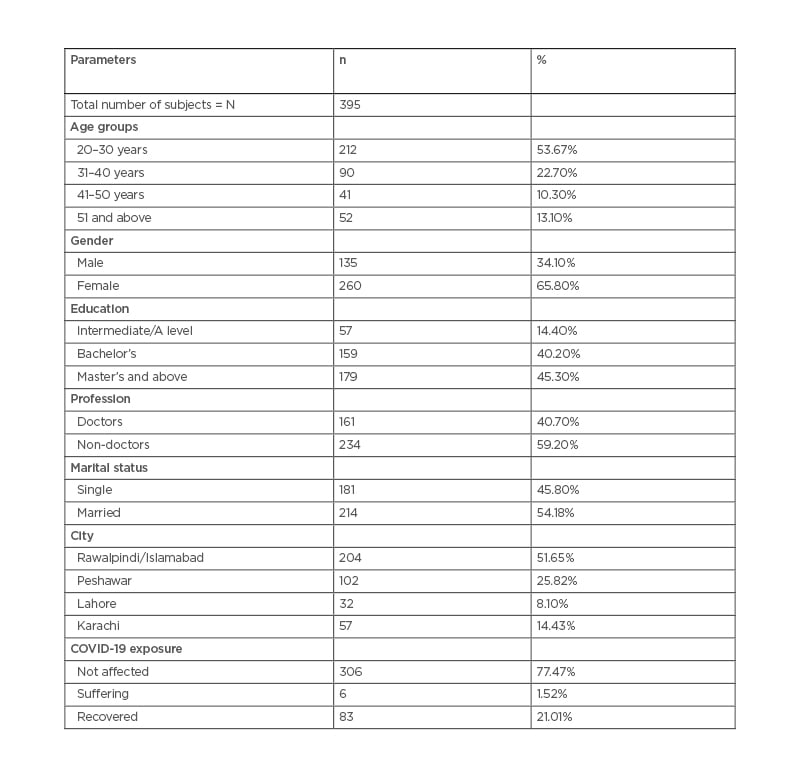
Table 1: Demographic profile of survey participants.
Among the participants, 148 (37%) did not suffer from anxiety while 38 (10%) reported having high or extreme levels of anxiety scores. Twenty-three (14%) doctors suffered from a moderate level of anxiety, which was a lower percentage compared to non-doctors (52: 22%). The proportion of moderate and extreme anxiety in females was 22% and 13%, respectively. Thirty-nine (22%) unmarried respondents had moderate anxiety, while 19 (10%) had extreme self-reported anxiety. Out of all the participants, 115 (38%) stayed at minimal anxiety levels after suffering from COVID-19 (Table 2).
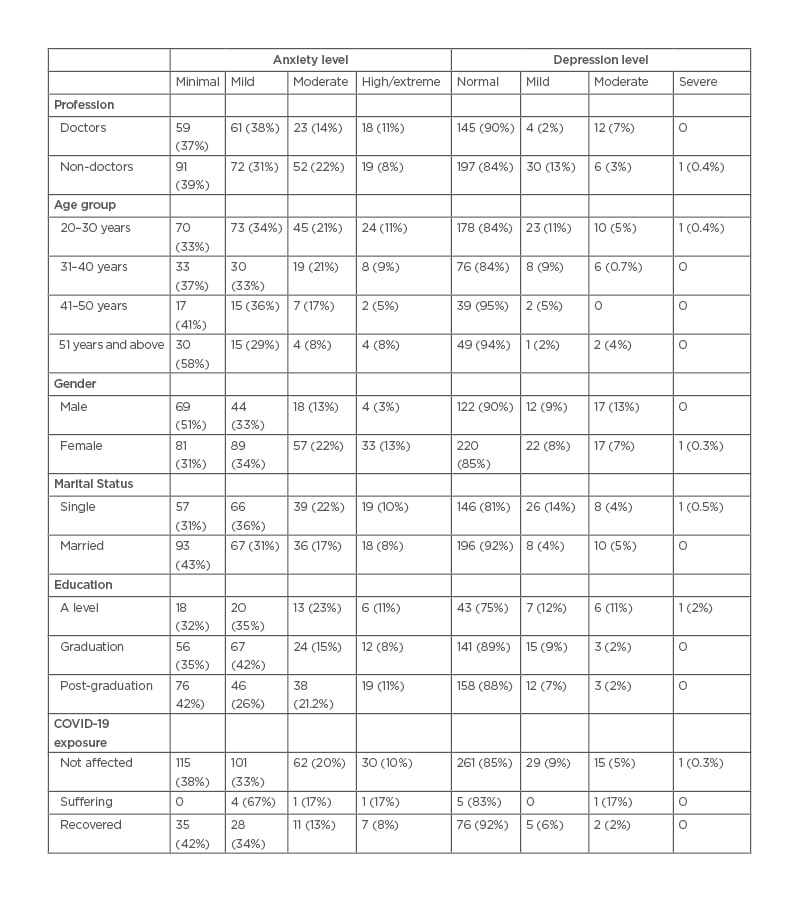
Table 2: Anxiety and depression levels in different groups.
A score indicating severe depression was observed in one respondent. Ninety per cent (n=145) of doctors and 85% (n=197) of non-doctors were found to have normal scores on SDS. A moderate level of depression was seen in 17 (13%) males. Five per cent (n=10) of married respondents had moderate depression, while 4% (n=8) had severe depression. Amongst the participants who had been affected by COVID-19, three were found to be moderately depressed compared with 15 (5%) moderately depressed individuals from the group who had not been affected (Table 2).
Table 3 reports the median SAS and SDS scores in different groups. The median SAS score was 11 for both doctors and non-doctors (range: 0–34). However, the median SDS score in doctors was significantly lower than in non-doctors (p=0.01). A statistically significant difference in SAS and SDS scores was observed in respondents from different age groups (p<0.001). It was found that the median SAS score of the 20–30 year age group (13) was significantly higher than the SAS score of respondents 50 years and above (median: 7.5). A similar trend was seen in the SDS scores of the two age groups (p=0.005). Females had significantly higher levels of anxiety and depression than males (p<0.001). Both scores differed in participants of different marital statuses (p<0.001). Unmarried participants had a median SAS score of 13 and a median SDS score of 37, while the scores for married people were 9 and 31, respectively. No significant difference was observed in the anxiety and depression scores of respondents from different cities, or with different educational backgrounds. Being infected with COVID-19 did not cause a significant difference in the SAS or SDS scores of this group compared to the group not affected by the virus.
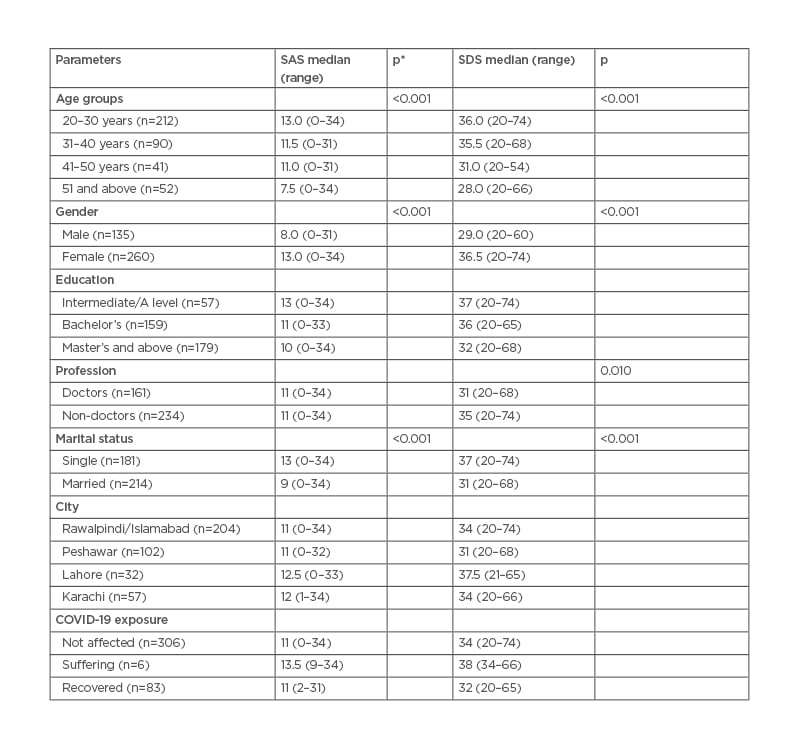
Table 3: Zung Self-Assessment Anxiety Score and Self-Assessment Depression Score. *Only significant values mentioned in the table. Confidence interval: 95%.
SAS: Zung Self-Assessment Anxiety Score; SDS: Self-Assessment Depression Score.
DISCUSSION
After inflicting critical physical impairment globally, the COVID-19 pandemic is now being associated with causing major emotional and mental health issues, leading to an increase in the prevalence of psychological distress, frustration, anxiety, depression,21-23 sleep disturbances, and even suicide in certain cases.24 Society’s mental health is being adversely affected by these factors. Approximately 35% of people were reported to be psychologically affected during the pandemic in a comprehensive study from China.25 An extensive study from Turkey reported relatively high levels of anxiety and depression (45.1% and 23.6%, respectively) in the general population during the pandemic.26
The aforementioned emotional and mental health issues have become overwhelming public health challenges all over the world. Medical healthcare workers, including paramedic staff, nurses, and doctors, who are directly exposed to patients with COVID-19 are more susceptible to acquiring infection and developing psychological distress compared with the rest of the general population.27,28
The authors’ findings showed that among all participants, 10–18% reported having moderate to extreme levels of anxiety. Similarly, 5–8% of respondents reported having mild to moderate depression scores. They observed that there was no significant difference between anxiety levels of doctors in comparison to non-doctors. On the contrary, depression levels were significantly higher in non-doctors compared with doctors. The results were in accordance with multiple studies that have identified signs of mental distress, anxiety, and depression among the general population in wake of the COVID-19 pandemic.29 Some studies suggest that the fear of contracting the infection and uncertainties regarding the severity and outcome of the disease have produced extreme consequences related to the psychological wellbeing of the general population.30 Pakistan appears to be a victim of such fears and uncertainties, and the results of this study support this idea. Misinformation, false data, and failure to understand and follow preventative guidelines have contributed to increasing levels of stress and anxiety among the general population.31
The authors’ findings revealed that there was a significant difference in anxiety and depression levels between different age groups (p<0.001). The anxiety scores of the 20–30-year-old group were significantly higher than that of the 50-year-old and above group. Similarly, depression levels were also found to be higher in younger age groups when compared with older age groups (p=0.005).
The authors’ findings are consistent with the findings of Ahmed et al.32 and Gao et al.,33 who reported that respondents belonging to the younger age group (<40 years) exhibited more anxiety and depressive symptoms compared with older age groups. The main contributory factor is exposure to social media as it is the main source of information for younger people.33 Moreover, university and college students were also found to be more at risk of developing depression and anxiety when compared with other occupations, due to encountering situations like postponement of examinations, and unfamiliarity with online teaching methods.34 Disturbance in academic sessions has not only affected student performance and grades but has also caused struggles in trying to adapt to new teaching strategies. This rapid change in the learning environment is also adding to anxiety and depression.34 A cross-sectional study from Ireland reported anxiety levels of around 28% among the general population; the most vulnerable group liable to develop anxiety and depression was the younger age group.35
This study also found that females displayed significantly higher levels of anxiety and depression than males (p<0.001). These findings were consistent with that of Lei et al.36 and Mazza et al.,37 who reported a similar trend concerning the difference in anxiety and depression levels between males and females. The main reason is females’ susceptibility to experiencing more psychological distress and post-traumatic signs and symptoms.36,37 In contrast, a comprehensive study from the UK reported that males were associated with less probability of anxiety and depression despite experiencing a high mortality rate during the pandemic.38
These results displayed a significant difference in depression and anxiety scores between marital statuses (p<0.001). Unmarried participants exhibited significantly higher levels of anxiety and depression compared with married respondents. Emerging evidence has suggested that being single, divorced, or widowed can be one of the predictive factors for the development of anxiety and depressive symptoms, owing to a greater incidence of experiencing loneliness and lack of psychological support.36 On the contrary, one study has reported high anxiety levels in married participants in compared with single respondents.33
The authors recognise a few limitations of the study. The study was carried out when the pandemic was at its peak. Lockdown made it impossible to conduct a face-to-face survey. Thus, further research is recommended post-lockdown to remove any biases concerning subjectivity and reliability. Secondly, no comparison was made to the incidence of anxiety and depression in the participants before COVID-19 in this study. The influence of pre-existing anxiety and depression on the outcome of the study should also be examined in post-COVID-19 analysis.
CONCLUSION
The current study concluded that doctors and non-doctors displayed signs of anxiety correspondingly. Consequently, signs of depression were prevalent among non-doctors compared with doctors during the pandemic. The groups most affected by anxiety and depression among the public included females, single participants, and adults from younger age groups.