INTRODUCTION
Ureteral double J (DJ) stent placement and replacement are common urological procedures,1 typically performed in the operating room under general or locoregional anaesthesia.2 The advent of single-use cystoscopes has enhanced the manoeuvrability and efficiency of endourological procedures.3,4 Therefore, elective DJ stenting could benefit from a modified approach to reduce patient medicalisation and the number of surgical interventions.5 This study aimed to evaluate the feasibility, safety, and patient satisfaction of DJ ureteral stenting using a flexible, disposable cystoscope under local anaesthesia (LA).
MATERIALS AND METHODS
The authors analysed prospectively collected data from all patients who underwent DJ stent insertion or replacement using a flexible, single-use cystoscope under LA between February 2022–April 2024 at two tertiary referral centres in Italy and England. Technical failure was defined as the inability to complete the scheduled procedure for positioning or replacing the ureteral stent. A visual analogue scale (VAS) was used for pain scores (range: 0–10, where 10 represented worst pain experienced). Patient satisfaction with the procedure and willingness to undergo future LA ureteral stenting were also inquired.
RESULTS
A total of 177 consecutive procedures were performed, comprising: unilateral stent changes (n=122; 68.9%), unilateral stent insertion (n=22; 12.4%), bilateral stent changes (n=28; 15.8%), and bilateral stent placements (n=5; 2.8%). The median age, Charlson Comorbidity Index, and hospital stay were 76 years (interquartile range [IQR]: 66–80), 8 (IQR: 6–12), and 0 days (IQR: 0–1), respectively (Table 1). Technical failure occurred in 13 (7.3%) cases (11 stent changes and two stent insertions). These failures were due to stent encrustation, unpassable ureteral strictures, or abnormal ureteral orifice anatomy due to malignancy, and were successfully managed by percutaneous nephrostomy or stent insertion under sedation. Complications included one Clavien-Dindo Grade III (0.56%) case of stent migration, which required ureteroscopy for repositioning, and 10 Clavien-Dindo Grade II (5.6%) cases of urinary infection. Overall, 88.1% (n=156) of patients were satisfied with LA ureteral stenting, and 89.8% (n=159) indicated they would be willing to undergo further LA ureteral stenting.
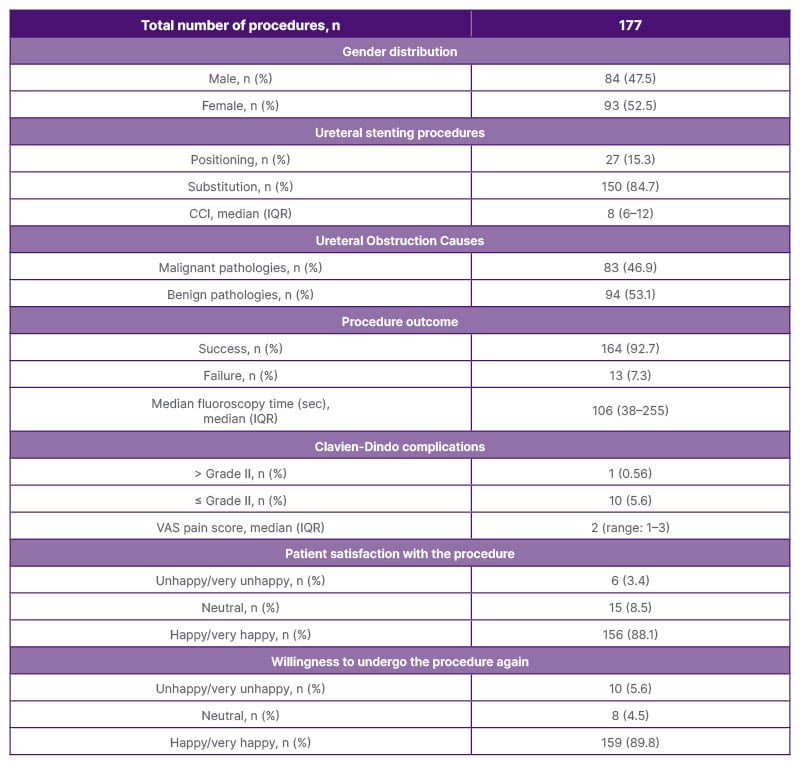
Table 1: Demographic features of the study population and their satisfaction with the procedure.
CCI: Charlson Comorbidity Index; IQR: interquartile range; VAS: visual analogue scale.
CONCLUSION
Results demonstrate that DJ stenting with a flexible dispensable cystoscope under LA in an outpatient setting is a feasible, safe, and well-tolerated procedure, even among elderly patients with multiple comorbidities. The procedure has a high success rate with low risk of minor complications. The risk of failure is associated with complex anatomy due to underlying pathologies or device encrustation. This approach enhances clinical efficiency, reduces anaesthesia-related risks, and may offer significant cost savings for healthcare systems.







