INTRODUCTION
Lower urinary tract symptoms (LUTS) in men are a growing problem as more men age. For a urological evaluation of LUTS in men, the International Prostate Symptom Score (IPSS) is the most frequently used questionnaire worldwide.1 The IPSS is intended to convert subjective symptoms into quantitative values, with questions on storage symptoms, irritative symptoms, and quality of life. The IPSS-scores are used for diagnosis, treatment choices, and evaluation of results.
However, several studies have shown problems regarding the completion of the IPSS.2,3 Self-completion resulted in an incomplete questionnaire in 53–73% of men.4,5 This, as well as poorer accuracy of symptom representation when completing the IPSS, was especially true for lower levels of education.6-8
A partner or another family member can provide an inexpensive and uncomplicated solution for assisting questionnaire completion. However, the question is: what if the patient himself cannot provide input? This study investigates the reliability of IPSS for men with LUTS when filled out by the ones closest to them: their partners.
MATERIALS AND METHODS
The study received approval from the local ethics committee. A power of 34 was calculated, and 43 couples were included. Men over 50 years of age attending the urology outpatient clinic were asked to participate. After approval, the individual and their partner were asked to separately fill out the IPSS for the man’s complaints. If the man came to his appointment alone, after approval, the partner (relationship >1 year, at least 3 nights a week together) was called to answer the questions by phone. Individual questions, total scores, and subscores (obstructive and irritative) were compared. For statistics, Pearson and Spearman correlation, Bland-Altman plotting, and Kappa were calculated in SPSS version 25.0.
RESULTS
A Pearson and Spearman correlation between patients’ and partners’ total scores proved 0.62 and 0.61, respectively. Bland-Altman plotting showed substantial spread, and Kappa was 0.162 (slight). As men had higher scores, partners tended to score higher as well. As shown in Table 1, 20 couples (46.5%) scored the patient’s symptoms in the same severity category (mild [n=5], moderate [n=23], and severe [n=15]); 22 (51.2%) differed in one category; and one couple (2.3%) differed in two categories. Partners tended to slightly overscore, and therefore, seemed only moderately able to assess true symptom severity. Even for quality of life, partners proved only modestly reliable (Kappa 0.192). The irritative subscore proved slightly better assessed than the storage subscore, mainly because of the question on nocturia, which showed a fair correlation with a Kappa of 0.367.
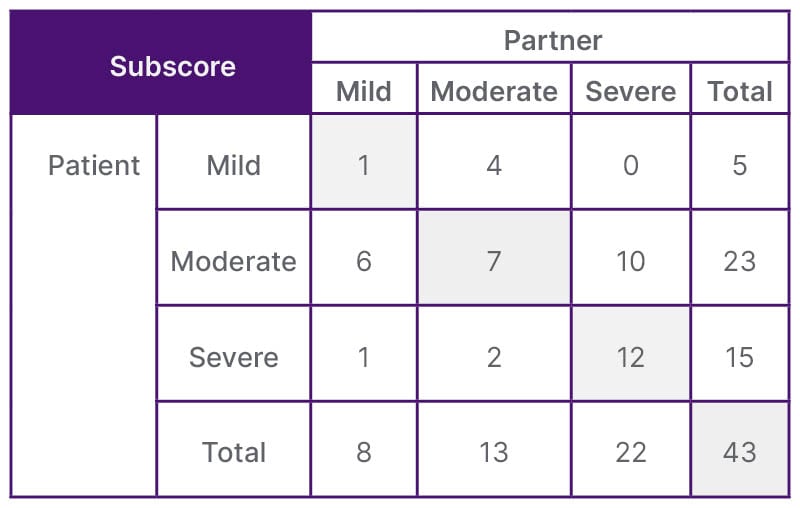
Table 1: Correlation between International Prostate Symptom Scores completed by the patient himself and the scores completed by the partner on the male lower urinary tract symptoms.
CONCLUSION
For the first time, a study was performed in which the IPSS scores of male LUTS was completed by their partners. Partners were found to be only modestly able to reliably replace their husbands. Considering that the sudden request for partners to fill out the form does not conform to the reality where the questionnaire is sent in advance, the partner’s result in that situation may be better than the result tested in the authors’ study. If the IPSS is not sufficiently understood, another instrument could possibly be used, as shown in previous research.3,9 With an increase in men dependent on caregivers, especially those who are not as close as the spouses tested in this study, a reliable alternative assessment of symptoms by others is desirable.







