Abstract
Background: Acute portal vein thrombus (APVT) refers to the abrupt occlusion of the portal vein and often requires anticoagulation. Oesophageal varices may occur in patients with cirrhosis and APVT and may require endoscopic eradication. The timing of anticoagulation post-treatment remains a clinical challenge, with considerable variability in approach. The risk of rebleeding versus thrombus progression must be weighed, but no clear guidance on safe timing exists.
Purpose: This review aims to identify the safe timing for recommencing anticoagulation for APVT post-treatment of oesophageal varices in patients with cirrhosis.
Methods: Three databases, Cochrane, Embase, and PubMed, were searched with the terms “portal vein thrombus,” “oesophageal varices,” and “anticoagulation.” Out of 235 studies, five were eligible for review.Results: In 372 patients with APVT (across five studies), 25 (6.72%) experienced rebleeding at a median follow-up of 21 days. The most common anticoagulant was low molecular weight heparin (LMWH). The median time to recommence anticoagulation was 59 hours post-treatment after endoscopic band ligation. One RCT (43 patients) showed zero rebleeds at 14 days with nadroparin starting within 48 hours, followed by warfarin for 5 months.
Conclusion: Early recommencement of anticoagulation for APVT, particularly LMWH, within 59 hours post-endoscopic band ligation of oesophageal varices may be safe, with a low rebleed rate. Further research is required to address this clinically significant topic, with no definite guidance to date.
Key Points
1. Portal vein thrombosis occurs in up to 16% of patients with cirrhosis, and the risk increases with severity. Oesophageal varices are common in cirrhosis. Optimal timing for restarting anticoagulation after variceal bleeding remains unclear, highlighting the need to balance thrombosis and rebleeding risks.
2. This literature review includes five studies, over 6 years, across 415 patients, aimed at identifying the safe timing of recommencing anticoagulation in patients with acute portal vein thrombus and treated oesophageal varices.
3. Commencement within 59 hours post-treatment of oesophageal varices, primarily with low molecular weight heparin, carries less risks of rebleeding at 21 days and may be safe, but the area requires ongoing research.
INTRODUCTION
Portal vein thrombus (PVT) is characterised by narrowing or blockage of the portal vein by a blood clot. Obstruction may be complete or partial. Acute PVT (APVT) occurs with abrupt portal vein occlusion and is defined as symptom duration under 60 days and absence of collateralisation features.1 Chronic PVT is often asymptomatic and has features of portal hypertension and collateralised circulation. The most common cause of PVT is liver cirrhosis, and in patients without cirrhosis, the main causes are inherited or acquired prothrombotic states. PVT is reported in up to 16% of patients with cirrhosis. Treatment options for PVT include anticoagulation with low molecular weight heparin (LMWH) or novel oral anticoagulants, thrombolysis, and transvenous intrahepatic portal shunt placement.2
Another common complication of liver cirrhosis is oesophageal varices. At the time of diagnosis, 30% of patients with cirrhosis have varices and this progresses to 90% at 10 years. Oesophageal varices occur due to portal hypertension, leading to portocaval anastomoses in an effort to decompress the portal system. Collateral vessels slowly enlarge and connect the systemic and portal venous systems.3 The modified Paquet’s classification of oesophageal varices is one method used to endoscopically classify the severity of varices: microcapillaries located in the distal oesophagus or oesophagogastric junction (Grade I), one or two small varices located in the distal oesophagus (Grade II), medium-sized varices of any number (Grade III), and large-sized varices in any part of the oesophagus (Grade IV).4
Endoscopic treatment of bleeding oesophageal varices includes endoscopic variceal ligation and sclerotherapy, typically performed for Grade III and IV varices. In 10–20% of patients, rebleeding may occur.5
In patients with both APVT and oesophageal varices, the timing of recommencing anticoagulation for APVT, after haemostasis of oesophageal varices, remains a question with no definitive guidance. Given the critical need to balance the risk of rebleeding and progression of PVT, this topic remains pertinent for review.
AIM
This literature review aims to identify the safe timing for recommencing anticoagulation in patients with APVT and treated oesophageal varices, by reviewing recent literature and assessing outcomes including rebleed from anticoagulation and death.
METHODS
Three databases, Cochrane, Embase, and PubMed, were searched with MeSH terms ([‘portal vein thrombus’] AND [‘oesophageal varices’] AND [‘anticoagulation’]). A total of 235 studies were identified, and after applying inclusion and exclusion criteria, five studies were suitable for inclusion (Figure 1 and Table 1).6–10
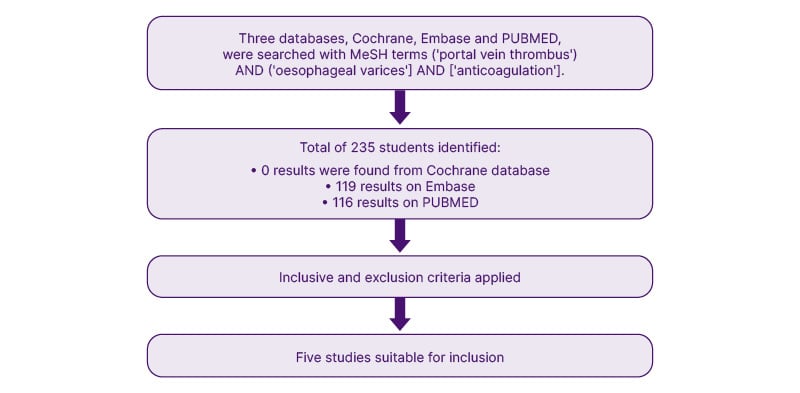
Figure 1: Search methodology.
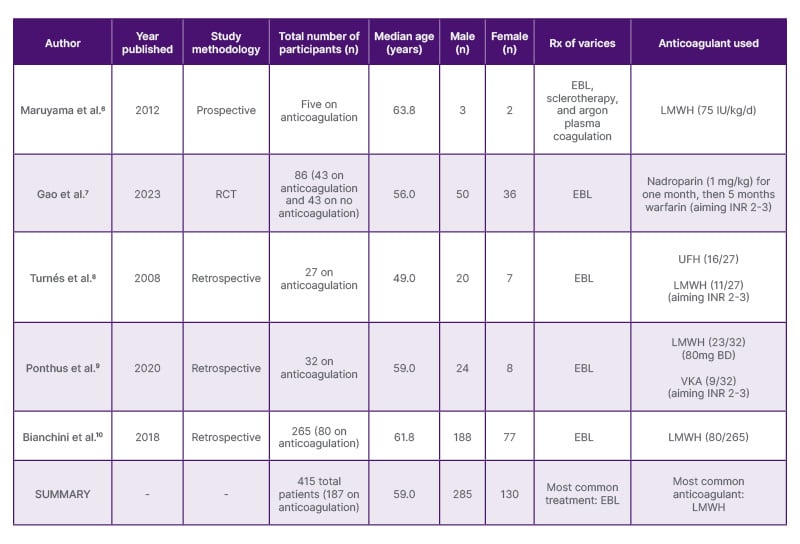
Table 1: Characteristics of the five included studies.
BD: twice a day; EBL: endoscopic band ligation; INR: international normalised ratio; LMWH: low molecular weight heparin; RCT: randomised controlled trial; Rx: treatment; UFH: unfractionated heparin; VKA: vitamin K antagonist.
Studies were included with the following criteria: if they were in English, randomised controlled trials, systematic reviews, observational studies, studies examining the timing of anticoagulation, studies with adults more than 18 years of age, liver cirrhosis, endoscopically treated oesophageal varices, portal vein thrombosis and given anticoagulation, studies examining oesophageal variceal rebleeding events, and death from rebleeding events.
Studies were excluded with the following criteria: if they were not in English; participants with chronic PVT; studies that did not address the timing of anticoagulation post-varix treatment; studies with participants less than 18 years of age; participants with untreated oesophageal varices, non-anticoagulation treatment of APVT, or experienced anticoagulation for conditions other than APVT; and participants who were pregnant.
Study Characteristics
The studies included are all somewhat recent (within the last 10 years), relatively similar regarding the age of patients (median age: 59 years), and show a relatively even distribution of male and female participants (285 [68.6%] were male and 130 [31.3%] were female), as well as the use of endoscopic band ligation (EBL) and the type of anticoagulant used (mostly heparins). There is variance in methodology, with only one study being a RCT and therefore representing the most robust methodology. All the remaining studies are retrospective. This may be related to the challenging nature of this topic and the difficulty of performing an RCT due to risks to participants, including haemorrhage and death. Overall, within these limitations, the five included studies are broadly homogeneous.
RESULTS
A total of 235 studies were identified (zero results were found from the Cochrane database, 119 results on Embase, and 116 results on PubMed). After title and abstract screening, zero studies were suitable from Cochrane, zero studies were suitable from Embase, and five studies were suitable from PubMed (Figure 1).
Five studies were included for review. The median age was 59 years. A total of 415 patients were recorded for outcomes, of which 187 were on anticoagulation, all with APVT and oesophageal varices treated with EBL. Of the total, 285 (68.6%) were male and 130 (31.3%) were female.
Maruyama et al.6 performed a prospective study with five participants, administering LMWH. All five (100%) achieved recanalisation by day 11. At a median follow-up of 351 days, there were zero rebleeds or deaths.6 Gao et al.7 performed an RCT with a total of 86 patients, of which 43 were given nadroparin (for 1 month) and then warfarin (for 5 months). Of the 43 patients, 29 (67.4%) achieved recanalisation at 6 months. There was one rebleed at 4 weeks, two rebleeds at 6 weeks, and 8 rebleeds at 6 months. No patients died from rebleeding in their study.7 Turnés et al.8 performed a retrospective study with 27 participants, of which 16 received unfractionated heparin (UFH) and 11 received LMWH, both for a median of 15 days. Twelve participants (44.4%) achieved recanalisation at a median follow-up of 43 months. At a median follow-up of 4 months, four (14.8%) patients had variceal bleeding.
Ponthus et al.9 performed a retrospective study with 32 participants, of which 23 received LMWH and nine received a vitamin K antagonist (VKA), both dosed to maintain blood at an international normalized ratio of 2–3. Of the 32 participants, 12 participants (37.5%) had complete recanalisation at a median follow-up of 2 weeks. Seven (21.2%) had variceal bleed on anticoagulation.
Bianchini et al.10 performed a retrospective study with 265 participants, of whom 80 received LMWH, which was not withheld post-EBL. At a follow-up of 4 weeks, three (1.13%) on LMWH had a rebleed, two (0.75%) died on LMWH within 28 days (of whom one died within 48 hours), and zero (0%) deaths were due to rebleeds.
Overall, the most common form of variceal treatment was EBL. The most common anticoagulant used was LMWH. The median follow-up duration was 21 days. Of 107 patients recorded for recanalisation, 58 (54.21%) achieved recanalisation. The median time to recommence anticoagulation was within 59 hours post-EBL. A total of 25 patients (6.72%) experienced rebleed. No patients died due to rebleeding from anticoagulation (Table 1).
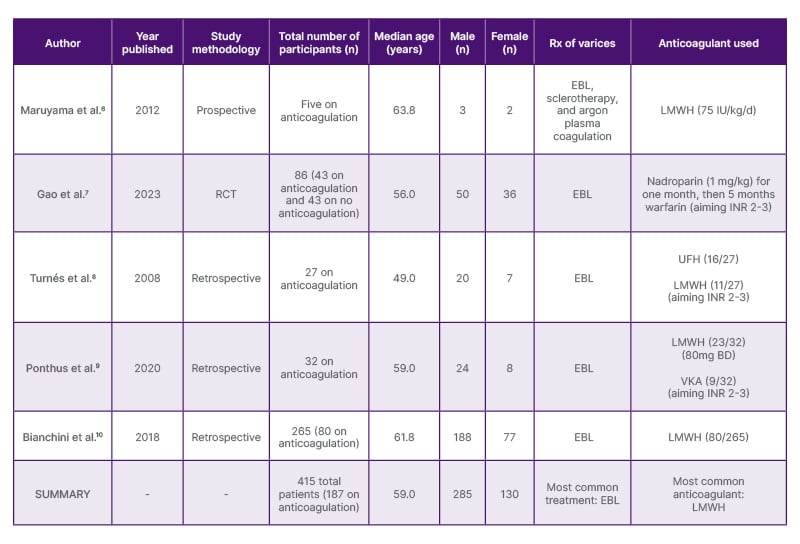
Table 1: Characteristics of the five included studies.
BD: twice a day; EBL: endoscopic band ligation; INR: international normalised ratio; LMWH: low molecular weight heparin; RCT: randomised controlled trial; Rx: treatment; UFH: unfractionated heparin; VKA: vitamin K antagonist.
DISCUSSION
No standardised treatment guideline exists for managing APVT in the setting of treated oesophageal variceal bleeding. A survey of 136 physicians in the United States demonstrated that 56% felt comfortable starting anticoagulation on their own and 40% referred to haematology. The most preferred anticoagulant was apixaban (47%), and 23% restarted immediately after EBL, 59% within 1 week, and 17% beyond 1 week post-EBL.11 There is considerable variation in the approach to managing anticoagulation in APVT and in patients treated for variceal bleeds, particularly with regard to timing.
This literature review aimed to understand the optimal timing of commencing anticoagulation in patients with APVT and oesophageal variceal bleeding. Overall, LMWH was the most commonly used agent, with a rebleeding rate of 6.72%. Most patients received EBL. The median time to recommence anticoagulation was 59 hours post-treatment of oesophageal varices.
The most robust literature from the five included studies was the RCT by Gao et al.7 They demonstrated that with the use of the regimen nadroparin calcium for 1 month and then 5 months of warfarin, the rate of rebleeding was 0% at 14 days. There was one rebleed at 4 weeks, two rebleeds at 6 weeks, and eight rebleeds at 6 months. No patients died from rebleeding in their study. 7
Nadroparin is a type of LMWH. It is not currently available in Australia. When a proposal was submitted for consideration of its use in venous thromboembolism prophylaxis, it was rejected for use in all patients by Therapeutic Goods Administration (TGA) in September 2018, due to lack of adequate representation of patient subgroups, including myocardial infarcts, unstable angina, and stroke.12
Odriozola et al.13 published a review article in 2022 discussing anticoagulant management of APVT with LMWH, UFH, VKAs and direct oral anticoagulants. With their four included meta-analyses, they demonstrated recanalisation rates (of any amount) from 66.6–71.5%. Early administration ranging from within 14 days to 6 months was found to be crucial for treatment success. There were major and minor bleeding rates (when compared to untreated patients) of 10.3–11.0%, with no increase in 5-day treatment failure rates or 6-week mortality rates. However, there were no data correlating differences in bleeding outcomes post-EBL based on subacute, acute, and delayed commencement of anticoagulation.
Artaza et al.14 performed a retrospective cohort study (in 2018) involving 32 patients with cirrhosis and PVT. All patients received non-selective beta-blocker treatment or EBL. LMWH was given to 29 patients and VKA to three patients, aiming for an INR of 2–3. The median time to commencement of anticoagulation was 14 days. Sixteen patients commented within week 1, nine patients between weeks 2 and 3, and seven patients commenced beyond 3 weeks. Recanalisation was achieved in 23 patients (complete in 17 patients (53.1%) and partial in six patients (18.1%)). Three patients (9%) had haemorrhage, of which two were variceal rebleeds (one at 7 months and the other at 9 months), and one was brain haemorrhage (at 2 months). Overall, it was found that there were minimal rebleed rates when commencing LMWH within a median commencement time of 14 days.
Chen et al.15 performed a retrospective cohort study on 66 patients with PVT from 2002–2014. Thirty patients were on warfarin (2.5 mg daily, aiming INR of 2–3) and 36 patients did not receive any anticoagulation. Thrombus improvement was found in 15 (68.2%) patients on warfarin, remained stable in four patients (18.2%), and progressed in three patients (13.6%). Thirteen (43.3%) patients had anticoagulation within the first month, 12 (40%) from 1–3 months, and five patients (16.7 %) commenced after 3 months. The median time on anticoagulation was 7.6 months (range: 0.2–52.0 months). No patients underwent EBL earlier. There were six deaths (all in the non-anticoagulated group); four due to gastrointestinal bleeding, one due to renal failure, and in one the cause was undetermined. Regarding variance in timing of commencement of anticoagulation, there were no patient outcomes (such as haemorrhage or mortality) measured directly in relation to the change in timing, in this retrospective cohort study.
Amitrano et al.16 performed a retrospective cohort study of 39 patients with non-neoplastic PVT from 2005–2006. Twenty-eight patients received 200 U/kg/day of LMWH (enoxaparin) for a minimum of 6 months. Of these, 14 patients (50%) were also admitted with gastrointestinal bleeding. In this subgroup, LMWH was commenced after EBL was completed and a beta-blocker prescribed. The median time for LMWH commencement was 4 months. Of the 28 patients, complete recanalisation occurred in 33.3%, partial in 50%, and no improvement in 16.7%. There were no adverse events such as haemorrhage or death at a median follow-up time of 11 months (range: 7–17 months). Overall, there is considerable variation in the literature but no definitive guidance surrounding the timing of anticoagulation. It appears that relatively early anticoagulation may be safe in APVT and EBL-treated oesophageal varices, when using LMWH, resulting in low rate of rebleed. There may be a role for nadroparin that would require further investigation pertaining to patients with AVPT.
CONCLUSION
In conclusion, there is a lack of consensus regarding the safe timing of recommencing anticoagulation in patients with APVT, following treatment of oesophageal varices. On review of the literature, it appears that commencement within 59 hours post-treatment of oesophageal varices, primarily with LMWH, is associated with lower risks of rebleeding at 21 days and may be safe; however, this is not definitive without further investigation. Nadroparin may have a role and has been investigated with a robust RCT; however, it is not currently approved by Therapeutic Goods Administration (TGA) for use in Australia. Ultimately, further investigation into this topic is necessary, as it remains a contentious topic of clinical importance without clear guidance.