INTRODUCTION
Invasive pulmonary aspergillosis is a potentially life-threatening complication in immunocompromised patients, particularly solid organ transplant recipients.1 Lung transplant patients are at increased risk due to direct airway exposure, prolonged immunosuppressive therapy, and impaired mucociliary clearance. Long-term immunosuppressive therapy, critical for preventing graft rejection, also predisposes patients to opportunistic infections like aspergillosis.1 Although antifungal prophylaxis is routinely employed, breakthrough infections can occur, highlighting the diagnostic and therapeutic challenges involved in maintaining the graft function while treating an active infection.
METHODS
A 60-year-old man, with a history of COPD and previously treated Mycobacterium avium complex infection, underwent a bilateral lung transplantation in July 2024 after completing a thorough evaluation. The patient was maintained on tacrolimus, prednisone, and mycophenolate mofetil as standard immunosuppression, in addition to itraconazole for fungal prophylaxis per the authors’ center’s protocol.
RESULTS
In September 2024, two months after transplant, the patient developed worsening dyspnea, decreased pulmonary function, and pleural effusions. Chest CT showed bilateral effusions, nodular densities, and compressive atelectasis (Figure 1A). Bronchoalveolar lavage (BAL) confirmed Aspergillus flavus and a high galactomannan antigen level (4.9), necessitating a change in the antifungal prophylaxis to isavuconazonium. His course was complicated by recurrent pleural effusions, requiring chest tube placement, and the persistent growth of Aspergillus in BAL, prompting a change of antifungal therapy to voriconazole along with inhaled amphotericin.2 With combination therapy, careful adjustment of his immunosuppressive regimen to balance infection control and graft function, and adequate monitoring of antifungal levels, he showed remarkable radiological and symptom improvement (Figure 1B).3
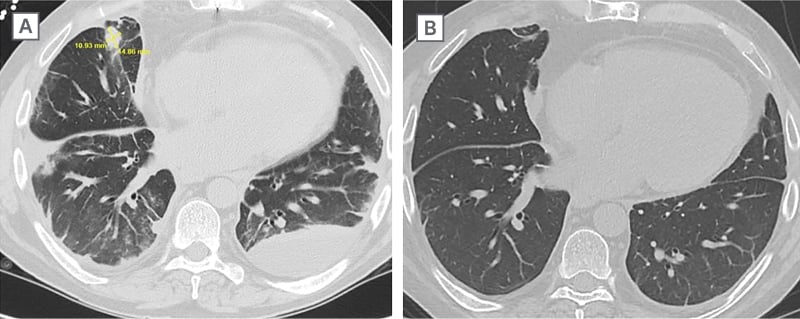
Figure 1: CT before and after treatment.
A) Initial CT showing bilateral effusions and nodular densities. B) CT after 3 months of treatment with voriconazole as well as inhaled amphotericin.
CONCLUSION
This case highlights the elevated risk of invasive pulmonary aspergillosis among lung transplant recipients, even when antifungal prophylaxis is implemented, emphasizing the significant risks associated with immunosuppressive therapy and the complexities involved in diagnosing and managing fungal infections in this vulnerable population. The immunosuppressive effects of tacrolimus and prednisone severely impair immune defenses, leading to fungal invasion. The interplay between immunosuppression, diagnostic uncertainty between infection and rejection, and limitations of standard antifungal prophylaxis with possible antifungal resistance require a multi-disciplinary approach. The use of BAL for direct identification and monitoring of galactomannan levels is essential for an early and accurate diagnosis. Individualized modulation of immunosuppression, in conjunction with combination antifungal therapy, was key to the clinical recovery of the patient.







