BACKGROUND
HIV causes immunodepression, which can lead to severe outcomes of COVID-19 infection. However, clinical studies have shown conflicting reports regarding outcomes of COVID-19 infection in patients with HIV. This National Inpatient Sample (NIS) study aimed to determine the impact of HIV on the severity of outcomes in patients with COVID-19 infection.1-3
METHODS
The authors identified patients hospitalized with COVID-19 infection who had a history of HIV using the 2020–2021 NIS database. STATA/MP 17.0 software (StataCorp, College Station, Texas, USA) was used for statistical analysis. Multivariate logistic regression analysis was performed.
RESULTS
There were 818,011 patients hospitalized with COVID-19 infection, and 36,232 patients hospitalized with a history of HIV. The patients with COVID-19 infection were stratified based on their HIV status. There were 815,979 patients with COVID-19 who did not have HIV, and 2,032 patients who had both COVID-19 and HIV (Table 1). White people constituted the largest ethnic group in the category of COVID-19 infection without HIV, while African American people constituted the largest ethnic group in the category of COVID-19 infection with HIV. Hispanic people constituted the second largest group in both categories. Patients in the lowest national income quartile and those with Medicaid insurance constituted the largest group among the national income quartile and insurance groups, respectively. The length of hospital stay among patients with COVID-19 and HIV was 10.4 days. For those without HIV, it was 8.2 days, with a p value of <0.001. The mortality rate was 13.1% among patients with COVID-19 but without HIV. For those with HIV, it was 13.3%, with a p value of 0.72. The unadjusted odds ratio (OR) of mortality in patients with COVID-19 and HIV was 1.02. The adjusted OR of mortality, after adjustment for age, sex, race, Charlson Comorbidity Index (CCI), national income quartile, and insurance, was 0.53, with a p value of <0.001. This indicated that the mortality rate among patients with COVID-19 and HIV was significantly lower than those without HIV (Table 2). The unadjusted OR of invasive ventilation in patients with COVID-19 and HIV was 1.26, while the adjusted OR was 0.50, with a p value of <0.001. This indicated that the need for invasive ventilation among patients with COVID-19 and HIV was significantly lower compared to those without HIV.
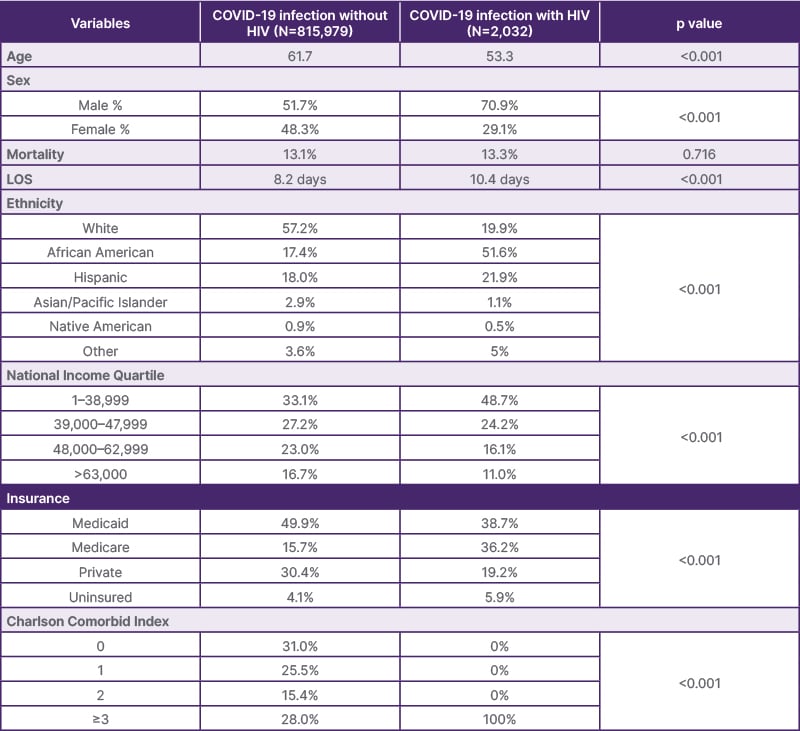
Table 1: Demographic and clinical characteristics, 2020–2021 National Inpatient Sample database.
LOS: length of stay.
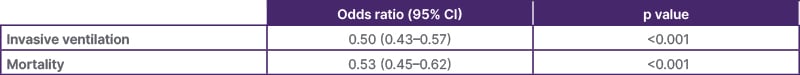
Table 2: Outcomes-adjusted odds ratio.
CONCLUSION
The authors’ analysis of the NIS database suggests that HIV was not a major risk factor for severe COVID-19 infection. Patients with COVID-19 infection and HIV had longer lengths of stay. However, they had a lower need for invasive ventilation and a lower mortality rate than those without HIV.







