RATIONALE
Plasma fibrinogen and C-reactive protein (CRP) are acute phase reactants that are increasingly being investigated as potential biomarkers for COPD severity, progression, and exacerbation risk.1,2 However, their roles across the full spectrum of spirometric disease severity, especially in pre-COPD, remain poorly understood. Emerging data suggest that the pre-COPD population, such as those in Global Initiative for Chronic Obstructive Lung Disease (GOLD) Stage 0 and preserved ratio impaired spirometry (PRISm), represent a heterogenous mix of individuals. Some individuals progress to develop milder disease (GOLD 1), while others progress to develop a more severe disease (GOLD 2–4) within the same timeframe.3 Yet, how fibrinogen or CRP levels vary across this continuum, particularly in pre-COPD, which is a stage marked by distinct progression patterns, remains unclear.
OBJECTIVE
The authors’ objective was to determine the distribution of plasma fibrinogen and CRP levels across the spirometric spectrum of pre-COPD and COPD.
METHODS
The authors conducted pulmonary function testing and respiratory health surveys among U.S. Veterans with a smoking history, with or without a COPD diagnosis, who were undergoing lung cancer screening at the San Francisco Veterans Affairs Health Care System.4 Blood samples obtained at the time of survey completion were tested for fibrinogen (using the Clauss method) and C-reactive protein (CRP; via high-sensitivity immunoturbidimetric assay). The authors examined fibrinogen and CRP distributions across GOLD stages and analysed their associations with respiratory exacerbation frequency using regression modeling, adjusting for age, sex, height, weight, and smoking status (current versus former) as well as smoking burden (pack-years).
RESULTS
Among 312 participants (96% male, mean age 70 years) with stable disease (no exacerbation for ≥6 weeks prior), 40% had GOLD 0, 11% had PRISm, 20% had GOLD 1, 23% had GOLD 2, and 7% had GOLD 3 or 4. As previously reported,4 the frequency of moderate/severe exacerbations increased with advancing spirometric disease.
Fibrinogen levels were 367±83, 407±72, 354±73, 386±83, and 391±68 mg/dL for GOLD 0, PRISm, GOLD 1, GOLD 2, and GOLD 3/4, respectively. Participants with PRISm had higher fibrinogen levels compared to GOLD 0 and GOLD 1 (Figure 1A and 1B). In severe COPD (GOLD 3 and 4), higher fibrinogen trended toward more frequent exacerbations, while in participants with PRISm, higher fibrinogen showed a trend toward fewer exacerbations (p=0.08; Figure 1C). CRP levels were 5.0±7.7, 6.3±6.9, 3.0±4.1, 5.5±13.9, and 5.3±9.8 mg/dL for GOLD 0, PRISm, GOLD 1, GOLD 2, and GOLD 3/4, respectively, with no significant differences observed (Figure 1D–F). CRP levels did not show a significant trend with exacerbation risk. Notably, both fibrinogen and CRP appeared lowest in GOLD 1, although these differences were not statistically significant.
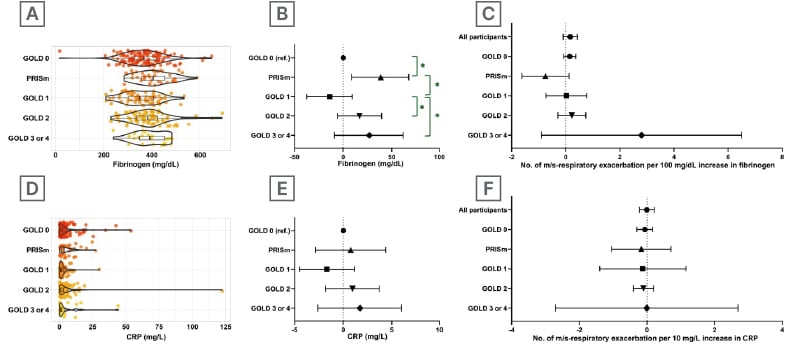
Table 1: Acute inflammatory markers in COPD spectrum.
A and D: Distribution of fibrinogen (A) and CRP (D) levels across the pre-COPD and COPD disease spectrum. B and E: Covariate-adjusted values of fibrinogen (B) and CRP (E). Values are presented as mean±95% CI. * and brackets indicate significant (p<0.05) comparisons. C and F: Associations between the number of moderate to very severe (m/s) respiratory exacerbations and levels of fibrinogen (C) or CRP (F) for each pre-COPD and COPD categories. Each line on Y-axis represents a separate regression. Values are presented as parameter estimate±95% CI. CRP: C-reactive protein.
CONCLUSION
Fibrinogen and CRP levels do not follow a linear trend across the COPD severity spectrum, possibly reflecting the underlying heterogeneity of pre-COPD and COPD. The lower levels of fibrinogen and CRP levels in GOLD 1 align with recent data suggesting that individuals who develop mild COPD (GOLD 1) may follow a different disease trajectory than those progressing to moderate or severe disease (GOLD 2–4).5
The higher fibrinogen level observed in PRISm, along with its inverse association with the exacerbation frequency, may reflect a systemic inflammatory phenotype that is not primarily driven by airway obstruction. This could represent underlying comorbidities such as obesity, metabolic syndrome, or cardiovascular disease, conditions that are more common in PRISm and contribute to systemic inflammation.6,7 Alternatively, it may indicate a distinct pathobiological pathway in PRISm, in which extrapulmonary factors such as vascular remodeling or restrictive physiology, play a greater role than classic airflow obstruction.
The lower levels of fibrinogen and CRP levels in GOLD 1 align with recent data suggesting that individuals who develop mild COPD (GOLD 1) may follow a different disease trajectory than those progressing to moderate or severe disease (GOLD 2–4).5
The higher fibrinogen level observed in PRISm, along with its inverse association with the exacerbation frequency, may reflect a systemic inflammatory phenotype that is not primarily driven by airway obstruction. This could represent underlying comorbidities such as obesity, metabolic syndrome, or cardiovascular disease, conditions that are more common in PRISm and contribute to systemic inflammation.6,7 Alternatively, it may indicate a distinct pathobiological pathway in PRISm, in which extrapulmonary factors such as vascular remodeling or restrictive physiology, play a greater role than classic airflow obstruction.







