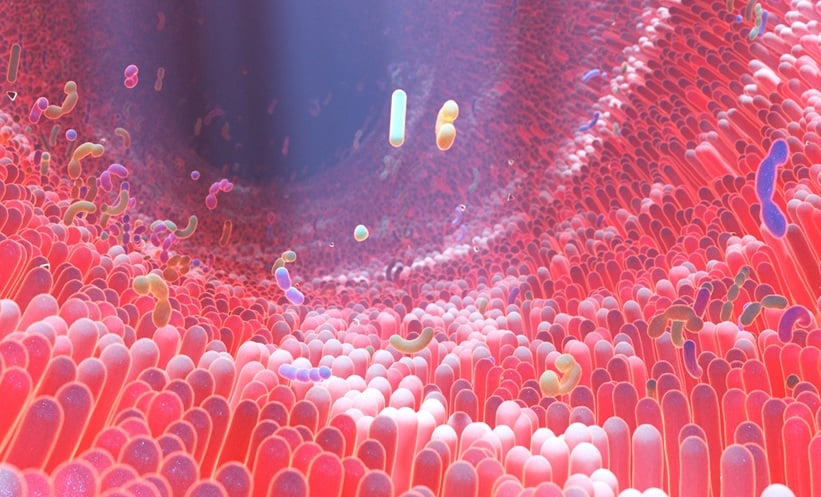
CHOLINE, betaine, and carnitine are dietary amines found in foods such as red meat, eggs, seafood, soy, cauliflower, milk, and whole grains. These compounds are metabolised by intestinal bacteria into trimethylamine (TMA), which is then transported to the liver and converted into trimethylamine-N-oxide (TMAO).
Elevated plasma levels of TMAO have been linked to increased risk of cardiovascular problems by promoting atherosclerosis and thrombosis, as well as impairing blood vessel function. Additionally, TMAO has been implicated in liver and kidney disease, diabetes, and other metabolic complications, suggesting it may contribute to worsening outcomes in patients with metabolic dysfunction-associated steatotic liver disease (MASLD).
In patients with advanced chronic liver disease (ACLD), several factors such as diet, changes in gut bacteria, and disruption of the gut–vascular barrier can lead to altered levels of TMA and TMAO. Research shows that during early, compensated stages of liver disease, TMAO levels tend to be higher, likely due to relatively preserved liver function and reduced shunting of blood away from the liver, which allows normal conversion of TMA to TMAO. However, as liver disease progresses, liver function declines and abnormal blood flow can cause TMA to bypass the liver, increasing TMA levels in the blood while reducing TMAO production.
In a recent study comparing patients with compensated and decompensated ACLD to healthy controls, higher TMAO levels were observed in the compensated group, though this was not statistically significant. Importantly, elevated TMA levels were independently associated with worse liver-related outcomes, including disease decompensation, liver transplantation, and death. This suggests that TMA may serve as a marker of liver disease severity.
The study also explored relationships with metabolic conditions like diabetes and obesity but found no clear association between TMAO levels and these factors in this cohort. Limitations included the retrospective design and small sample size, which affect the generalisability of the findings.
Overall, these results highlight the complex role of TMA and TMAO in chronic liver disease and underline the need for larger, prospective studies to clarify their potential as prognostic markers and targets for therapy, especially in early-stage liver disease.
Reference
Bürki JT et al. Exploring the trimethylamine pathway in advanced chronic liver disease. npj Gut Liver. 2025;2:15.