Abstract
Percutaneous coronary intervention (PCI) of coronary bifurcation lesions remains one of the most technically challenging procedures in interventional cardiology due to the complex anatomy and diverse lesion characteristics. These lesions account for approximately 15–25% of all PCI cases and are associated with higher rates of restenosis and adverse clinical outcomes compared to non-bifurcation lesions. Despite advancements in stent technology and procedural techniques, managing bifurcation lesions requires a tailored strategy that considers patient factors, lesion morphology, operator expertise, and outcome goals. This review introduces the Patient, Lesion, Operator, Technique, and Outcomes (PLOTO) framework, an innovative, algorithmic, and systemic approach to bifurcation PCI. Emphasis is placed on lesion assessment, including Medina classification, bifurcation angle, calcification, and imaging guidance, and the choice between provisional and two-stent strategies. Practical recommendations and evidence from contemporary studies are integrated to guide optimal procedural planning and execution, aiming to simplify complexity while enhancing clinical results.
Key Points
1. Coronary bifurcation lesions are challenging and are associated with higher rates of restenosis and stent thrombosis when compared to non-bifurcation percutaneous coronary intervention (PCI), particularly following complex procedures.2. Simplifying the procedure as much as possible and limiting the number of implanted stents by using a stepwise provisional strategy remains the recommended strategy for the majority of bifurcation PCI.
3. In this review article, the authors propose the Patient, Lesion, Operator, Technique, and Outcomes (PLOTO) framework to approach bifurcation PCI, which focuses on the five titular components. This model aims to tailor interventions to individual patient needs and help select the most appropriate technique to optimise outcomes.
INTRODUCTION
Coronary bifurcation lesions pose a significant challenge in interventional cardiology, accounting for approximately 15–25% of all percutaneous coronary interventions (PCI).1,2 These lesions arise at arterial branching points, creating anatomical complexities that complicate intervention and increase the risk of side branch (SB) occlusion. Clinically, bifurcation lesions are associated with higher rates of restenosis and stent thrombosis when compared to non-bifurcation PCI, particularly following complex procedures.1-3Despite the development of second-generation drug-eluting stents and advancements in procedural strategies, bifurcation PCI remains technically demanding due to factors such as heterogeneous plaque distribution, complex flow dynamics, and the need to preserve both main branches and SBs.4-6Given these ongoing challenges, there is a critical need for practical, strategy-driven approaches that simplify bifurcation interventions without compromising efficacy.7 Hence, this review aims to bridge complexity and clarity by offering a streamlined, real-world approach to PCI of bifurcation coronary lesions.To facilitate a more effective and simplified approach to bifurcation PCI, the authors developed the Patient, Lesion, Operator, Technique, and Outcomes (PLOTO) framework (Figure 1), an innovative, simplified, and systemic approach that focuses on five key components. This model emphasises a holistic view, tailoring interventions to individual patient needs and lesion characteristics, and selecting the most appropriate technique to optimise outcomes. By integrating these factors systematically, the authors aim to provide a clearer and more practical roadmap for navigating the complexities inherent in bifurcation interventions.
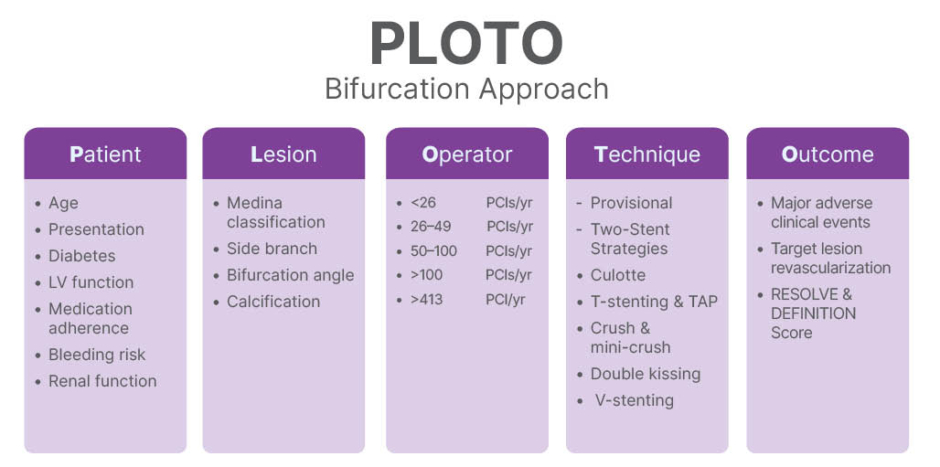
Figure 1: The Patient, Lesion, Operator, Technique, and Outcomes (PLOTO) framework for percutaneous coronary intervention of coronary bifurcation lesions.
LV: left ventricular; PCI: percutaneous coronary interventions; PLOTO: Patient, Lesion, Operator, Technique, and Outcomes; TAP: T and small protrusion; yr: year.
THE PATIENT
When approaching a bifurcation lesion, many patient-related factors should be considered, as they may affect the technique and equipment being used.8 Those factors include:
- Patient age: Operators might simplify the approach in older patients, minimising contrast and time in the catheterisation laboratory.
- Patient presentation, acute coronary syndrome versus stable ischaemic heart disease: A provisional approach might be preferred by some operators in unstable patients presenting with acute coronary syndrome with less than thrombolysis in myocardial infarction (TIMI) 3 flow. More complex techniques might be more appealing in stable patients.
- Diabetes: Patients with diabetes tend to have worse outcomes. In young people with diabetes who have left anterior descending bifurcation lesions, surgical consultation should be considered.
- Left ventricular function: Mechanical support devices may be considered in patients with left ventricular ejection fraction <35%, especially for left main (LM) or last conduit bifurcation disease.
- Medication adherence: Simple bifurcation techniques may reduce stent thrombosis risk in patients with questionable compliance.
- Bleeding risk: Minimising stent deployment may be advisable in patients with high bleeding risk needing possible interruption of antiplatelet therapy.
- Renal function: Simple techniques and reduced contrast use are preferred for patients with advanced kidney disease.
THE LESION
Definition
According to the Bifurcation Academic Research Consortium (Bif-ARC)9 and the European Bifurcation Club consensus,10 coronary bifurcation includes a coronary region consisting of three major parts: 1) the proximal main vessel; 2) the distal main vessel (DMV); and 3) the SB. The longest and largest distal branch should be designated the DMV given the linear relationship between diameter, length, flow, and supplied myocardial mass.
Angiographically, a bifurcation lesion is defined as a coronary stenosis adjacent to and/or involving an adequate-sized SB (≥2.0 mm in reference diameter). The lesion is considered significant when its % diameter stenosis is >50% and the minimum luminal diameter in at least one of the three segments is located ≤4 mm from the point of bifurcation.9-12
Lesion Assessment
Accurate assessment of the bifurcation lesion not only dictates the selection of the ideal technique but can also influence clinical outcomes. The following four factors form the foundation of bifurcation lesion assessment.
Medina classification
The Medina classification13 evaluates the location of atherosclerotic disease by assigning a score of 1 to any lesion involving the proximal main vessel, DMV, or SB with ≥50% stenosis. The Medina classification is widely accepted as a universal classification for bifurcation lesions.9,14
Bif-ARC identifies ‘true’ bifurcation lesions, involving a significant (≥50%) diameter stenosis both in the main vessel and SB (i.e., Medina 1, 1, 1; 1, 0, 1; or 0, 1, 1), and ‘non-true’ lesions in all other cases. Bif-ARC also recommends classifying the bifurcation lesions in LM and non-LM bifurcations, in addition to SB size and atherosclerotic involvement.9,15,16
Side branch
Accurate evaluation of the SB is critical in bifurcation PCI planning, as it strongly influences the choice between provisional and two-stent strategies.8,9,17 SB should be defined as ‘relevant’ if symptoms are stemming from a large amount (>10%) of ischaemic SB-related myocardium, impacting prognosis.9 Key factors include SB diameter (>2.5 mm), lesion length (>5–10 mm), ostial stenosis severity (≥70%), and TIMI flow post-main vessel intervention. Longer or heavily diseased SBs are at higher risk of occlusion, can be more challenging, and may warrant upfront two-stent techniques.18 Physiologic measurements such as fractional flow reserve and instantaneous wave-free ratio can guide the need for SB intervention after main vessel stenting.19 Intravascular imaging supports SB assessment by evaluating plaque burden and guidewire positioning in addition to post-PCI assessment.20
Bifurcation angle
Bifurcation angle plays a pivotal role in guiding PCI strategy.8,17,21,22 A wide bifurcation angle (>70°) is associated with a higher risk of SB occlusion, carinal shift, and difficulty in re-crossing the SB, favouring an upfront two-stent technique. Conversely, a narrow angle (<70°, particularly <50–60°) may favour provisional stenting (PS).8,22
Calcification
Calcification significantly increases procedural complexity and is associated with higher risks of stent under-expansion, SB compromise, and adverse clinical outcomes.8,9 It is a key feature of complex bifurcations, often necessitating advanced lesion preparation techniques and sometimes favouring a planned two-stent strategy.10,14
THE OPERATOR
Bifurcation PCI is challenging and requires many steps. Operator comfort and expertise with a chosen technique strongly influence procedural success and patient outcomes. Previous studies have shown an inverse relationship between PCI operator volume and in-hospital mortality that persisted in risk-adjusted analyses.23 Other studies also showed that PCI performed by experienced operators during complex PCI was independently associated with lower long-term risks of cardiac death.24 Specifically for LM bifurcation studies, patients who underwent LM PCI by high-volume and experienced operators had better short- and long-term prognoses.25 Therefore, Bif-ARC recommends reporting the volume of LM bifurcation PCI per year in the centre. In this article, the authors will use the same definition of experienced operators as previously applied in the paper by Fanaroff et al.23 Operators performing <50 PCIs annually are defined as low-volume operators.26 Operators performing 50–100 and >100 PCIs per year are defined as intermediate- and high-volume operators, respectively. Extreme high- and low-volume operators are defined as those performing >413 PCIs (97.5th percentile of the volume distribution) and <26 PCIs (2.5th percentile of the distribution) annually, respectively.23
THE TECHNIQUE
Simplifying the procedure as much as possible and limiting the number of implanted stents by using a stepwise provisional strategy remains the recommended strategy for the majority of true LM and non-LM bifurcation PCIs.8,10 Table 1 summarises the essential targets that should be pursued during bifurcation PCI.
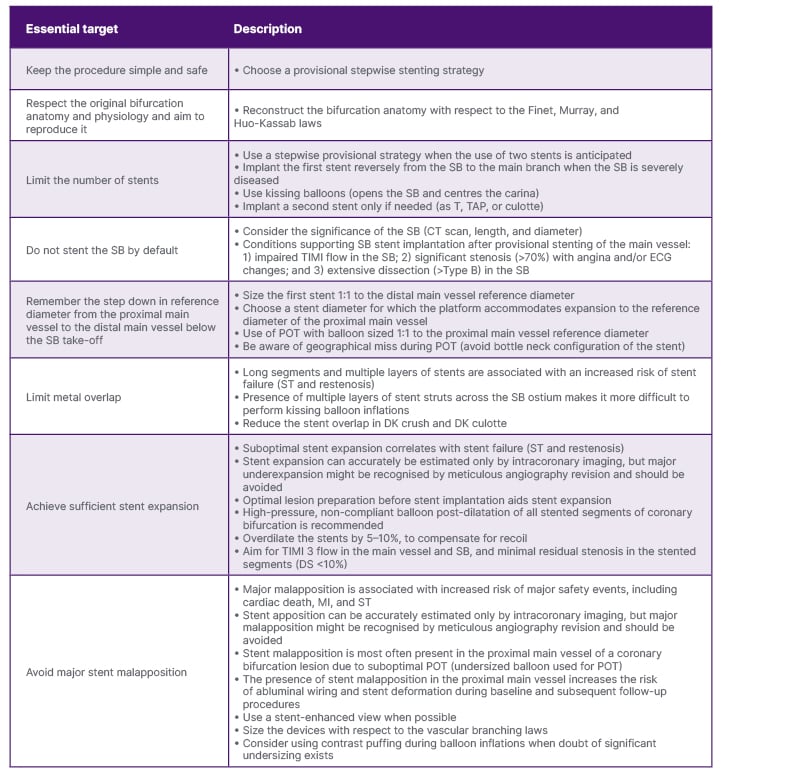
Table 1: Key principles of bifurcation percutaneous coronary intervention promoted by the European Bifurcation Club.
Adapted from Burzotta et al.10
DK: double-kissing; DS: diameter stenosis; MI: myocardial infarction; POT: proximal optimisation technique; SB: side branch; ST: stent thrombosis; TAP: T and small protrusion; TIMI: thrombolysis in myocardial infarction.
Provisional Stenting
Provisional bifurcation stenting is the recommended default strategy for most bifurcation lesions,10,27 primarily due to its simplicity, safety profile, and efficiency. This is the preferred technique among many operators, especially low and intermediate volume operators.
The key procedural steps are (Figure 2):27-31
- Initial guidewire placement: Wiring both myocardial bridge (MB) and SB to maintain access and procedural flexibility.
- Main vessel preparation: Balloon pre-dilation to assess lesion compliance and likelihood of plaque shift.
- Main vessel stenting: Deploy drug-eluting stent across SB ostium, ensuring lesion coverage without unnecessarily compromising SB.
- Proximal optimisation technique (POT): Using a short balloon in proximal MB to improve stent apposition and facilitate SB access.
- Assessment of SB: Angiographic and/or physiologic assessment post-POT; intervention if compromised.
- Rewiring and SB dilation: If needed, crossing stent struts for balloon dilation and possibly kissing balloon inflation.
- SB stenting (if necessary): Techniques like T and small protrusion, T-stenting, or culotte depending on anatomy.
- Final POT and kissing balloon inflation: To optimise proximal stent segment and correct malapposition.
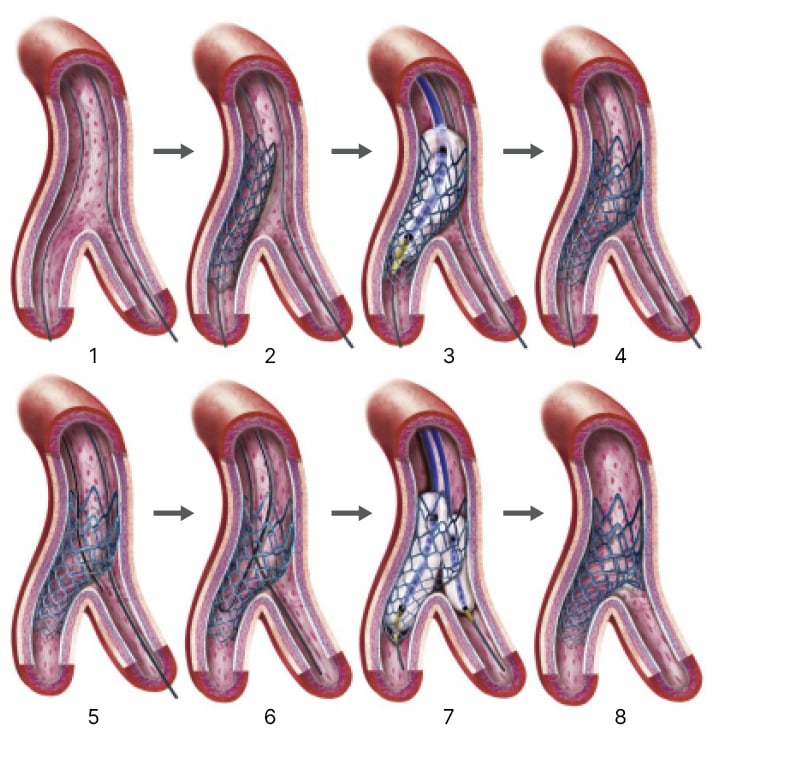
Figure 2: Step-by-step provisional side branch stenting.
Adapted from Sawaya FJ et al.27
Two-Stent Strategies
Two-stent strategies are used in coronary bifurcation lesions when the SB has significant disease, a large territory is at risk, or when provisional strategy fails. Multiple techniques have been developed, each tailored to specific anatomical and procedural needs:10
Culotte: For similar branch sizes and narrow angles; stenting one branch then the other with overlap in MB.
T-Stenting and T and small protrusion: For approximately 90° SB take-off; minimal protrusion into MB; a simple technique, but with a risk of incomplete coverage if the angle is suboptimal.
Crush and mini-crush: SB stentcrushed by MB stent, followed by kissing balloon inflation; mini-crush reduces metal layers.
Double kissing (DK) crush: Two rounds of kissing balloon inflation to optimise stent apposition; superior outcomes in distal LM bifurcations. There have been many modifications to the crush techniques over the years.32 The DKCRUSH-V trial showed superior outcomes of DK crush compared to PS in distal LM bifurcations (Figure 3).33
V-stenting: Simultaneous MB and SB stenting in wide angles with short main branches; efficient but limited to short lesions.
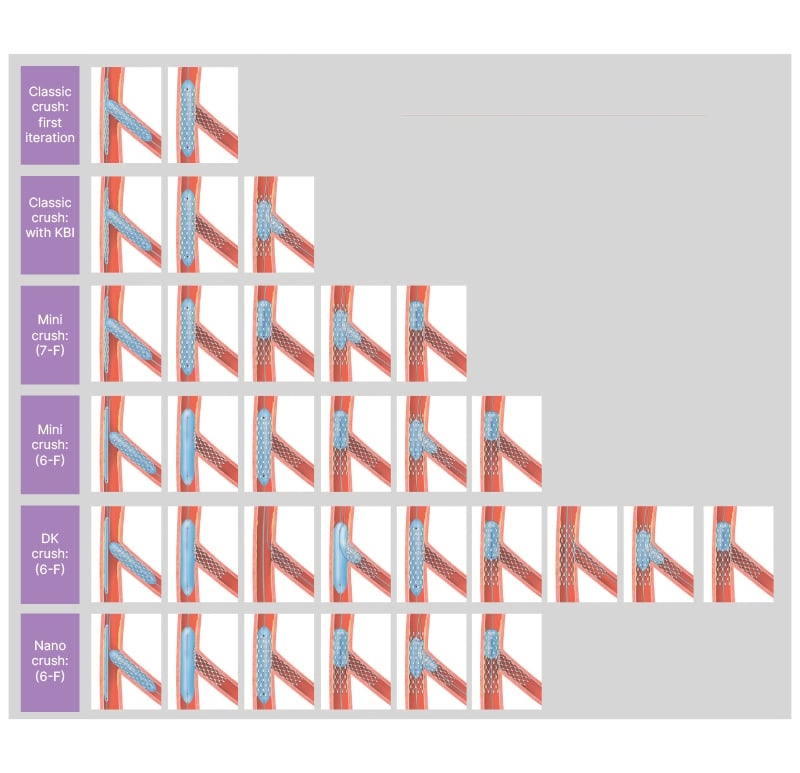
Figure 3: Evolution of the crush technique demonstrating stent deployment and final kissing balloon inflation.
Adapted from Raphael CE et al.32 DK: double-kissing; KBI: kissing balloon inflation.
Choosing the Best Technique
The provisional approach is recognised as the gold standard approach for the majority of bifurcation lesions.22,34 Yet, the use of two-stent implantation techniques is advised to treat selected patients with complex bifurcated lesions with relevant and significantly diseased SB.34 It is important to note that DK crush has many steps and can be challenging to perform.35 The DKCRUSH-V trial required the primary operators to have performed ≥300 PCIs per year for 5 years, including at least 20 LM PCIs per year, and operators had to demonstrate proficiency in the DK crush technique in 3–5 cases before being allowed to enrol patients.36 Similar to chronic total occlusion interventions, there is likely a learning curve before optimal outcomes are achieved with DK crush.35
THE OUTCOMES
The clinical outcomes of the above-mentioned techniques have been evaluated in several RCTs. However, the interpretation of the trials is challenging because of comparisons of different strategies and inconsistent findings.1 Overall, two-stent techniques were not significantly better than PS in terms of clinical outcomes. However, some analysis suggested that there might be benefits of a two-stent approach in selected patients with true bifurcation lesions, especially in the case of long SB lesions.1
A pairwise meta-analysis including 18 RCTs1,7,33,36-51 comparing provisional stenting versus two-stent techniques (5,022 patients) did not show any difference between the two groups regarding major adverse clinical events (MACE; odds ratio: 1.19; 95% CI: 0.90–1.58; p=0.23) or any secondary outcomes. In this analysis, significant heterogeneity was observed between the RCTs regarding MACE, myocardial infarction, and target lesion revascularisation (TLR). To reduce heterogeneity, a meta-regression, using the mean SB lesion length as a continuous covariate, was performed. This showed lower rates of the primary endpoint (MACE) associated with the two-stent technique in the RCTs that had enrolled patients with longer SB lesions (estimate of 0.06; 95% CI: 0.02–0.10; p=0.002; residual heterogeneity Q: 17.07; p value for residual heterogeneity=0.15). This effect was apparent in the RCTs with a mean study-level SB lesion length >11 mm.1
When only RCTs enrolling patients with true bifurcations were considered,33,36,40,41,44-51 the analysis demonstrated a significant benefit from two-stent techniques in terms of MACE (OR: 1.52; 95% CI: 1.08–2.13; p=0.02), mainly driven by a higher risk of TLR following PS.1
In a network meta-analysis comparing all techniques to each other, DK crush was associated with significantly lower event rates than all other bifurcation stenting strategies regarding the primary endpoint (OR: 0.47; 95% CI: 0.36–0.62), as compared to PS, the second-best strategy in terms of MACE and TLR.1 Moreover, DK crush was related to a lower risk of myocardial infarction and stent thrombosis compared to all other techniques, except for T-stenting. However, the rate of cardiac death with DK crush was comparable to that of other bifurcation PCI techniques.1
Despite these advances, bifurcation PCI is still associated with a lower procedural success rate and worse clinical outcome compared with non-bifurcation PCI.27 Multiple risk scores have been introduced that mainly focused on lesion-related factors and the procedural techniques that determine clinical outcome. The Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion (RESOLVE) score was established to evaluate the risk of SB occlusion.52 The Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts (DEFINITION) criteria were designed to establish a stratification system that could guide optimal stenting strategy.53 In an analysis of 5,537 patients from the BIFURCAT registry, clinical features were predominant predictors for hard endpoints, and lesion features were predominant for predicting lesion-oriented clinical outcomes such as TLR and target vessel failure.54
CONCLUSION
This paper presents a referenced guide designed to assist interventional cardiologists in developing efficient strategies for bifurcation PCI. The proposed PLOTO framework serves as a tool to standardise decision-making and treatment planning, thereby supporting the achievement of optimal clinical outcomes. Continued research is encouraged to evaluate the long-term impact and effectiveness of implementing this methodology in clinical practice.







