Abstract
Eruptive xanthomas present as a sudden eruption of multiple yellow papules and are often associated with extreme hypertriglyceridaemia. Several reports describe eruptive xanthoma as the sole presenting symptom of unrecognised hypertriglyceridaemia in adults, but only a few cases report eruptive xanthoma associated with both unrecognised hypertriglyceridaemia and undiagnosed Type 2 diabetes. This report highlights the importance of identifying a cutaneous marker suggestive of an underlying metabolic disorder. A 34-year-old Filipino male presented with a 2-month history of sudden onset of multiple skin-coloured to yellowish papules on the extremities and trunk. He reported a strong family history of diabetes, hypertension, and premature cardiovascular death. Dermoscopy and histopathology were consistent with xanthoma. Referral to endocrinology and subsequent laboratory evaluation revealed severe dyslipidaemia, with triglyceride levels elevated to 1,989 mg/dL (approximately 13 times the upper limit of normal) and a fasting blood glucose of 13.7 mmol/L. After 16 weeks of pharmacologic therapy and lifestyle modification, the patient showed complete resolution of lesions, with normalisation of lipid and glucose levels and no recurrence. This case illustrates the critical role of dermatologic findings in the early detection of systemic metabolic disorders. Early multidisciplinary intervention is key to successful treatment and prevention of life-threatening complications.
Key Points
1. Recognising eruptive xanthomas can expedite the diagnosis of severe metabolic disease.2. In skin of colour, dermoscopy is a valuable tool to aid in the diagnosis, as the typical yellow hue of xanthomas may be less evident.
3. Early initiation of lipid-lowering and antidiabetic medications combined with lifestyle modification can result in rapid resolution of skin lesions and normalisation of metabolic parameters.
INTRODUCTION
Eruptive xanthoma is considered a rare disease with an incidence of 18 out of 100,000. It can only be seen in 10% of patients with severe hypertriglyceridaemia.1 There is no age or gender bias.2 It is important to promptly recognise this disease because it is a marker of severe hypertriglyceridaemia, which, if left untreated, will lead to increased risk of the potentially fatal complications of acute pancreatitis and atherosclerosis.3 A number of reports describe eruptive xanthoma as the primary presenting symptom of unrecognised hypertriglyceridaemia in adults; however, only a few reports document its association with both unrecognised hypertriglyceridaemia and undiagnosed Type 2 diabetes.4 This report aims to highlight the importance of early recognition of a cutaneous marker ofsevere metabolic disease.
CASE DESCRIPTION
A 34-year-old Filipino male smoker with a known history of hypertension, currently not on medication and without a known history of diabetes, presented to the dermatology outpatient department with a 2-month history of suddenly appearing, symmetrical, skin-coloured to yellowish papules on the arms, thighs, and trunk (Figure 1A). The patient had a Fitzpatrick skin Type IV. The lesions were associated with mild pruritus. There was no recent history of insect bite or contact with possible allergens. Review of systems revealed weight gain for the past 6 months, polyuria, polydipsia, polyphagia, and prickling sensation on hands and feet. There were no similar lesions in the family, but there was a strong family history of hypertension, diabetes, and death of a paternal grandfather at the early age of 50 years due to aneurysm. The patient worked as a truck driver and led a sedentary lifestyle. No prior consultation or intervention had been undertaken.
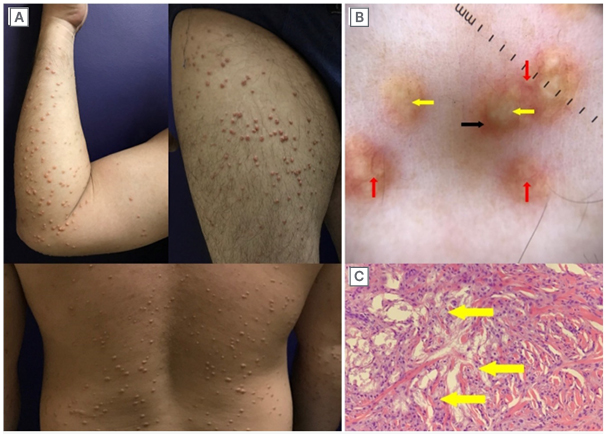
Figure 1: Images showing (A) lesions at baseline on the arms, thighs, and posterior trunk; (B) dermoscopy (10x); and (C) histopathology (left arm; haematoxylin and eosin stain).
A) Clinical picture of symmetrical skin-coloured to yellowish papules on arms, thighs, and trunk.
B) Dermoscopy findings of eruptive xanthoma (left arm, 10x magnification) showing a homogeneous yellow centre, some with
coalescing yellow globules in clusters (yellow arrows) surrounded by erythematous to hyperpigmented halo (black arrow), some with occasional serpentine vessels (red arrows).
C) Histopathology of eruptive xanthoma (left arm, H&E stain) showing variably-sized aggregates of lipid-laden histiocytes or foamy histiocytes (yellow arrows).
H&A: haematoxylin and eosin.
Dermoscopy of the lesions revealed a homogenous yellow centre. Some lesions showed coalescing yellow globules surrounded by erythematous to hyperpigmented halo, while some exhibited occasional serpentine vessels (Figure 1B).
Histopathological examination of a skin biopsy from the left arm was consistent with xanthoma. It showed variably sized aggregates of lipid-laden histiocytes (foamy histiocytes; Figure 1C), located in the upper third of the dermis, admixed with lymphocytes. Foci of extracellular lipid were also observed. The patient was promptly referred to an endocrinologist for further laboratory workup and confirmation of the diagnosis of eruptive xanthoma.
Laboratory results revealed severe hypertriglyceridaemia at 1,989 mg/dL, which is 13-times higher than the normal value. Grossly cloudy serum was visible upon centrifugation of the patient’s blood. Very-low-density lipoprotein was also 10-times elevated at a value of 397 mg/dL, along with other lipid parameters (Table 1), supporting the diagnosis of severe dyslipidaemia.5 Fasting plasma glucose was also two-times elevated from the upper limit at 13.74 mmol/L, which confirmed the diagnosis of Type 2 diabetes.6
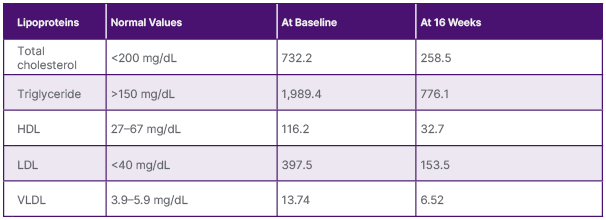
Table 1: Lipid panel of patient at baseline and at 16 weeks after treatment.
HDL: high-density lipoprotein; LDL: low-density lipoprotein; VLDL: very-low-density lipoprotein.
Unfortunately, HbA1c was not available at that time. Patient also satisfied four out of the five criteria of NCEP/ATP III-AHA/NHLBI (2005) for metabolic syndrome, with a waist circumference of 104 cm, triglycerides of 1,989 mg/dL, a blood pressure of 130/90 mmHg, and fasting glucose of 275 mg/dL.7
Correlating the clinical presentation and laboratory findings confirmed the diagnosis of eruptive xanthoma. The patient was started on the following tablets: fenofibrate 200 mg once daily, atorvastatin 80 mg once at night, metformin 500 mg three times daily, gliclazide 80 mg once daily, and linagliptin 5 mg daily. Lifestyle modifications were also advised, including a low salt, low fat, low carbohydrate diet, smoking cessation, reduced alcohol intake, regular exercise, weight monitoring, and referral to a nutritionist. The patient was also advised to avoid manipulating the lesions and to use mild emollients. As early as 4 weeks of medical management and lifestyle modification, there was noticeable rapid improvement in the lesions, with 80% flattening and darkening of the previously yellowish papules. After 16 weeks of therapy (Figure 2), all lesions were completely resolved, with no recurrence noted. Repeat laboratory results showed a marked decrease in lipoproteins, particularly triglycerides, from 1,989 mg/dL to 776 mg/dL. Fasting blood sugar also decreased from 13.74 mmol/L to 6.52 mmol/L. HbA1c level was 7.0%. No adverse effects were reported.
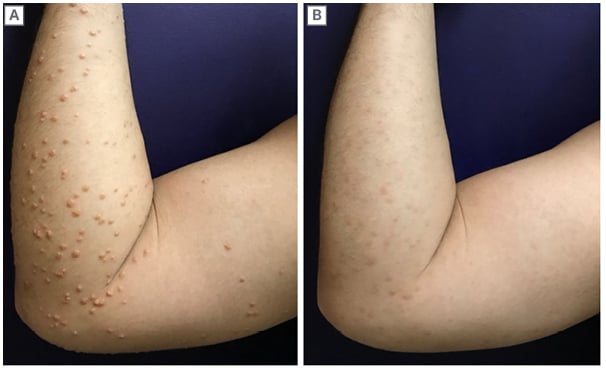
Figure 2: Comparison photos of arm at baseline and after 16 weeks.
Comparison photos from baseline at Week 0 (A) and after 16 weeks (B) of medical management and lifestyle modification.
DISCUSSION
In the literature, several reports describe eruptive xanthoma as the sole presenting symptom of unrecognised hypertriglyceridaemia in adults, but only a few cases document eruptive xanthoma associated with both unrecognised hypertriglyceridaemia and undiagnosed Type 2 diabetes.4,8-10 These cases involved seemingly healthy adults whose chief complaint was the appearance of yellowish papules, without other systemic symptoms.8-10 In contrast, the author’s case is notable because the lesions were not initially apparent due to the patient’s darker skin type with a yellow undertone.11 Although one published case report describes eruptive xanthoma in a Filipino adult, that patient initially presented with generalised body weakness and weight loss, with xanthomas appearing later in the course.12 In the author’s case, however, the primary symptom was the sudden eruption of yellowish papules without other systemic symptoms.
The pathogenesis of xanthoma begins with increased local extravasation of lipids through the blood vessel walls into the interstitial spaces of connective tissue. Macrophages subsequently engulf these lipid particles, resulting in the formation of foam cells, or lipid-laden macrophages. These foam cells then accumulate in the skin and tendons, leading to the development of xanthomas.1
According to the Frederickson Classification of Dyslipidemia, eruptive xanthoma variant is commonly seen in those with Type I, IV, and V dyslipidaemia. However, this classification relies only on the biochemical profiles and does not distinguish between the genetic or acquired causes of dyslipidaemia.13 In the recent classification of Berberich and Hegele13 regarding biochemical levels for dyslipidaemia in adults, the current case can be classified as having severe deviation, with triglycerides >885 mg/dL and low-density lipoprotein >194 mg/dL.13 This cut-off is important because most clinicians observe eruptive xanthoma at a triglyceride level of >1,000 mg/dL.1 At this state, the aetiology can be due to polygenic predisposition plus secondary factors such as diabetes and metabolic syndrome. Hence, family members should be screened for mixed hyperlipidaemia, diabetes, and obesity.In recent years, there has been a growing prevalence of lipid disorders among Southeast Asian populations, such as Filipino adults. The notable increase in cases may be attributed to rapid urbanisation, lifestyle changes, and a dietary shift toward Westernised food.14 Hence, in this case, it is more likely that both genetic and acquired causesare present.
In obesity and diabetes, the decrease in peripheral insulin resistance leads to lipolysis, decreased lipoprotein lipase, and defective chylomicron clearance. The combination of these mechanisms leads to a number of lipid disorders, including chylomicronaemia, hypertriglyceridaemia, increased low-density lipoprotein,and increased very-low-densitylipoprotein, which ultimately leads to xanthoma formation.1
Aside from eruptive xanthoma, the patient is also at risk for long-term atherosclerotic cardiovascular disease, hyperlipidaemic acute pancreatitis, and lipaemia retinalis.13 Hence, hyperlipidaemia requires immediate intervention to prevent thesedevastating consequences.
Interestingly, it remains unclear whether the severity of dyslipidaemia correlates with the number of eruptive papules. For example, the author’s current case with a baseline triglyceride level of 1,989 mg/dL exhibited widespread lesions across the extremities and trunk. This contrasts with another report in which a patient had a significantly higher triglyceride level of 7,157 mg/dL, but presented only a few lesions localised to the extensor extremities.2 The authors think these variations suggest that, while high triglyceride levels are associated with eruptive xanthomas, the exact relationship between triglyceride levels and the number and distribution of lesions remains poorly defined.
Moreover, the authors think that the characteristic yellowish hue of the papules may be difficult to appreciate in skin of colour (Figure 1A, bottom). With the aid of dermoscopy, the contrast between the homogeneous yellow centre and the hyperpigmented to erythematous periphery facilitates clinical diagnosis.8 Correlation of the histopathology result and metabolic panel confirmed the diagnosis oferuptive xanthoma.
In terms of management, eruptive xanthoma responds rapidly once the underlying dyslipidaemia has been addressed, often as early as 4 weeks, as seen in the authors’ case and in other reported cases (Table 2).2-3,15-17 However, if the underlying disorder is not treated, there is a high risk of developing acute pancreatitis and atherosclerosis, two potentially life-threatening complications.17
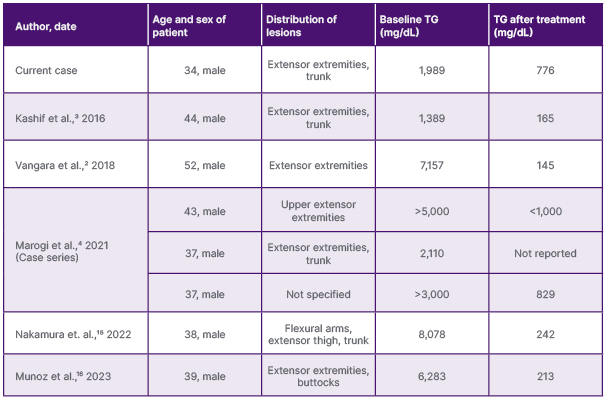
Table 2: Some of the previously reported eruptive xanthoma cases with severe hypertriglyceridaemia.
TG: serum triglycerides level.
CONCLUSION
In summary, eruptive xanthoma is an important cutaneous red flag of profound hypertriglyceridaemia, which may stem from either genetic causes of dyslipidaemia or secondary factors, such as poor glycaemic control in this patient. Improvement of dyslipidaemia and blood glucose through medications and lifestyle modification resulted in significant improvements in both metabolic parameters and skin lesions.
Early recognition by the dermatologist and timely referrals to an endocrinologist and nutritionist played a vital role in preventing potentially severe complications.
Patient Perspective
I am glad I had my skin rashes checked because I learned that I have some hidden medical problems. As the breadwinner of our family, I got scared of the consequences if no intervention was done. So, I am very thankful the treatment worked immediately.







