Abstract
Background: People with Type 2 diabetes (T2D) often have dyslipidaemia (72–85%). This study aimed to investigate the quality of care for blood lipid control in patients with T2D in Iran.
Method: In a cross-sectional retrospective study, the authors studied the quality of care provided to patients with T2D in 15 diabetes centres in five provinces of Iran. The PROCAM calculator was used to determine the low-density lipoprotein cholesterol (LDL-C) target levels based on patients’ cardiovascular risk scores. The suitability and rational prescribing of lipid-lowering drugs, medication errors, and achievement of target LDL-C levels based on individual patient needs were also assessed.
Results: The medical records of 2,500 patients were examined. The most commonly prescribed drug was atorvastatin (91.1%). Monotherapy was the preferred treatment option (68%). On average, 74% of the study population did not achieve individualised LDL-C target levels. The prescription of lipid-lowering drugs was not appropriate for the patients’ needs in the selected provinces. Inadequacy included no medication (approximately 23%) and insufficient medication therapy (approximately 17%) for patients with high LDL-C levels.
Conclusion: The study concludes that improved evidence-based prescription practices, enhanced performance of medical staff, continued medical education, and better medication management are needed to ensure improved lipid control in patients with T2D in Iran.
Key Points
1. This study reveals a critical mismatch in care, while low-risk diabetes patients had an 86% low-density lipoprotein cholesterol control rate, those at very high risk for heart attacks and strokes had a control rate of only 8–10%.2. The vast majority (74%) of patients failed to meet their lipid targets. Crucially, this was not solely due to poor adherence; 23% of uncontrolled patients received no lipid-lowering medication at all, and another 18% were prescribed insufficient doses, pointing directly to clinical inertia and suboptimal prescribing.
3. Treatment relied heavily on atorvastatin monotherapy (91%), with negligible use of guideline-recommended combination therapies like ezetimibe. Furthermore, the low-density lipoprotein-lowering effect of atorvastatin was suboptimal and not dose-proportional, and significant medication errors (e.g., irrational drug combinations) were identified.
INTRODUCTION
Diabetes is a chronic disease characterised by the body’s inability to use or produce sufficient insulin effectively. It is a growing global problem, with a higher disease burden in developing countries.1-4 In patients with Type 2 diabetes (T2D), one common group of abnormalities observed is diabetic dyslipidaemia, affecting 72–85% of these patients.5,6
Individuals with T2D are at a higher risk of developing cardiovascular diseases, stroke, and peripheral vascular diseases.1,7,8 This risk increases as low-density lipoprotein cholesterol (LDL-C) levels rise.9 Therefore, LDL-C levels are a vital aspect of treatment strategies for dyslipidaemia in patients with T2D.5,10-12
Significant clinical trials have demonstrated that lower LDL-C values are associated with a reduced risk of future cardiovascular events, with no lower limit identified for LDL-C levels.13,14 Although clinical studies have shown the safety of extremely low LDL-C levels, further monitoring is necessary.15,16
Updated guidelines, such as those of the American Diabetes Association (ADA), recommend an LDL-C goal of less than 100 mg/dL, while for patients with diabetes with established atherosclerotic cardiovascular disease, the target is less than 55 mg/dL.17
Like many other developing countries, Iran has a high prevalence of T2D, with recent studies estimating a significant increase of 45.5% in diabetes prevalence compared to 2016.18 Furthermore, the last national survey of risk factors for non-communicable diseases revealed that 15.14% of the Iranian population over 25 years old had diabetes in 2021.10
This study aimed to assess the quality of care in managing blood lipid levels among a representative group of patients with T2D in Iran. Specifically, the authors examined various aspects of prescribed medications, including patterns, rational use, and effectiveness, with a focus on achieving target LDL-C levels based on individual patient needs.
METHODS
Sample Size
This cross-sectional study was conducted in 15 diabetes centres across five provinces in Iran. Data were extracted from patients’ records in public, semi-public (centres related to the social security insurance organisation), and private centres. The selection of the diabetes centres and patients followed a cluster sampling method. Patients with a confirmed diagnosis of T2D, who were taking antidiabetic medications, had a comprehensive medical history from 2013–2017, and visited a doctor at least four times per year, were included in the study. The authors assumed that the adherence of these patients was in an acceptable range, >80%.19
Demographic information, laboratory examination results, prescription patterns, and treatment outcomes were extracted from the patients’ profiles in documentary and registry records.
The authors also focused on prescription patterns (the extent and profile of drug use), medication errors, achieving individualised targeting levels, and the effectiveness of lipid-lowering drugs in the T2D population.
PROCAM Calculator
The PROCAM calculator was used to determine LDL-C target levels based on patients’ cardiovascular risk scores. The PROCAM calculator is a reliable tool for predicting the 10-year risk of cardiovascular events based on a patient’s history and laboratory results. Eight components are checked, each with a different weight in the final calculation. These components include age, LDL-C, smoking status, high-density lipoprotein cholesterol, systolic blood pressure, family history of myocardial infarction, diabetes, and elevated triglyceride levels.15 The PROCAM score ranges from 0–87, with higher scores indicating a higher risk of cardiovascular disease.20
One important use of the PROCAM calculator is determining the target level of LDL-C in patients with diabetes. In this analysis, the authors used target LDL-C levels based on cardiovascular risk scores.
Rational Use of Medicines
Rational use of medicines means prescribing medications based on the patient’s needs, in appropriate doses, for an adequate period, and at the lowest cost to the community.21 In this study, the suitability and rational prescribing of lipid-lowering drugs were assessed using the defined daily dose (DDD).
Medication Errors
Medical errors are defined as preventable adverse events or mistakes that occur during the provision of healthcare services, resulting in harm to patients.22,23 These errors can occur at any point in the healthcare delivery process, including diagnosis, treatment, medication administration, surgery, and follow-up care.24 The authors investigated medication errors, including prescription errors such as medical interactions, duplication therapy, and dosing of LDL-C-lowering drugs.
Statistical Analysis
Statistical analysis was performed using the STATA software version 14 (Stata, College Station, Texas, USA). Continuous variables, such as lipid indices, were presented as mean and standard deviation. Categorical and binary outcomes, such as achieving the LDL-C targets and family history of myocardial infarction, were presented as proportions with a 95% CI. The statistical significance of LDL-C fluctuation during the period of use was examined using MANOVA analysis.
RESULTS
Demographic and Prescription Pattern
The study included 2,500 patients, of whom 521 were excluded due to incomplete records. Among the remaining 1,979 patients, the mean age was 62.3 years, with about 34% being older than 65 years. The demographic characteristics and prescribed lipid-lowering drugs are summarised in Table 1.
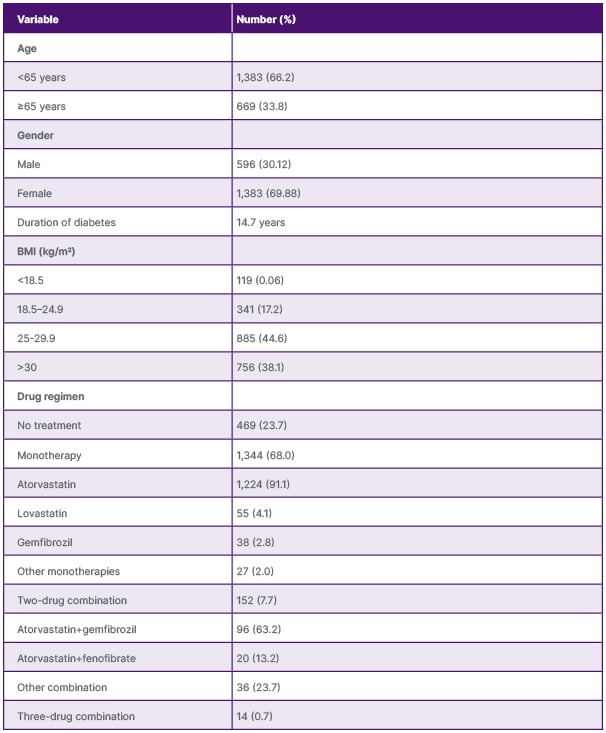
Table 1: Demographic characteristics and the frequency of prescribed lipid-lowering drugs in patients with Type 2 diabetes.
Table 1 also summarises the prescription pattern of lipid-lowering drugs in these patients. The most commonly prescribed drug was atorvastatin, received by 91.1% of the patients. Monotherapy was the preferred treatment option, with 68% of the patients receiving a single drug. Combination therapy was less common, with only 7.7% of the patients receiving two drugs and less than 1% receiving three drugs.
Achieving the Low-Density Lipoprotein Cholesterol Target
Table 2 presents key findings on the management of LDL-C across different provinces. It reveals that, on average, patients had an LDL-C level (88.80 mg/dL) that was higher than their recommended target (≤69.12 mg/dL). Consequently, only 26.06% of patients achieved their goal. Crucially, among those with uncontrolled LDL-C, the majority (59.7%) were already taking a sufficient daily dose of medication, indicating a potential gap in treatment efficacy or adherence.
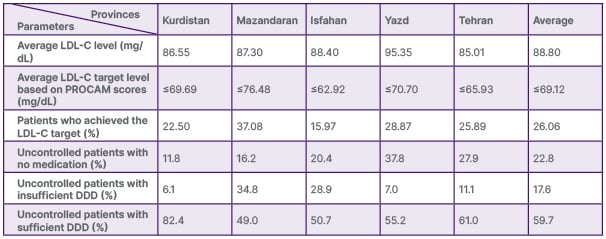
Table 2: Average low-density lipoprotein cholesterol levels compared to the average target levels based on Prospective Cardiovascular Münster Study score and lipid-lowering drug prescription status in patients with uncontrolled low-density lipoprotein cholesterol in selected provinces of Iran.
DDD: defined daily dose; LDL-C: low-density lipoprotein cholesterol; PROCAM: Prospective Cardiovascular Münster Study.
Table 3 provides a detailed analysis of LDL-C management among 1,979 Iranian patients with diabetes over 5 years. Patients are divided into five risk groups based on their PROCAM score, ranging from ‘low’ to ‘very high’. Each year, patients are categorised as ‘controlled’ (meeting their target) or ‘uncontrolled’ (missing their target). Each risk group has a specific, progressively lower LDL-C target, from <116 mg/dL for low risk to <55 mg/dL for very high risk. The final columns display the actual average LDL-C levels for patients in each risk group, broken down by five Iranian provinces.
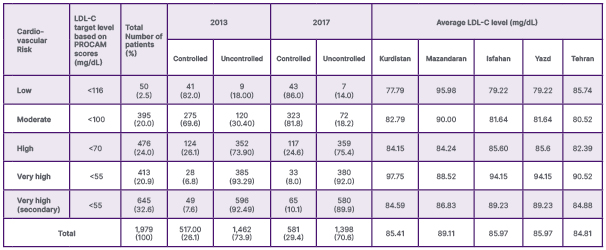
Table 3: The average low-density lipoprotein cholesterol levels in patients with diabetes over 5 years, compared to the target low-density lipoprotein cholesterol levels based on Prospective Cardiovascular Münster Study scores in the selected provinces.
LDL-C: low-density lipoprotein cholesterol; PROCAM: Prospective Cardiovascular Münster Study.
The comparison illustrates that none of the regions have achieved the optimal levels of cholesterol targets. The results showed that, on average, 74% of the study population did not achieve individualised LDL-C target levels.
Medication Errors
Medication errors can significantly affect the timely and effective treatment of patients. In this study, medication errors were investigated, including prescription errors such as medication interactions and duplication therapy. Among the study population, 1.06% had concomitant use of two fibrates or two statins without scientific justification. The consequent use of atorvastatin and lovastatin was the third most widely used drug combination in patients with T2D. Among the total research population, 9.58% of the patients simultaneously received two drugs from the drug categories of statins and fibrates. A few cases of simultaneous use of three drugs from these categories were also observed.
In addition, on average, 22.79% of patients with uncontrolled LDL-C levels did not receive any lipid-lowering medication, and 17.33% received insufficient daily doses, indicating errors in the prescribing decision (Table 2).
These medication errors can be attributed to improper monitoring of medication therapy by physicians.
Effectiveness of Drugs
The effectiveness of different doses of atorvastatin was evaluated in patients who had not taken any medication for their lipid disorder. The changes in LDL-C levels were compared between those who took atorvastatin and those who did not take any lipid-lowering drugs. The results are shown in Table 4.
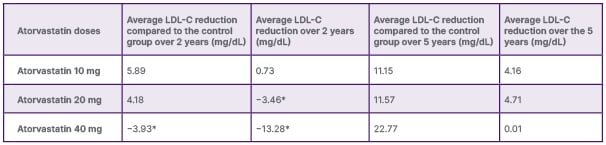
Table 4: Efficacy of different doses of atorvastatin in reducing low-density lipoprotein cholesterol with and without a control group.
*The negative numbers indicate an increase in LDL-C.
LDL-C: low-density lipoprotein cholesterol.
The results indicate that atorvastatin shows a reduction in LDL-C compared to the control group. However, the effects were not directly related to the prescribed doses, and the level of blood-lipid reductions was lower than expected.25,26
Rational Use of Medicines
The authors evaluated the appropriateness and rational prescription of lipid-lowering medications using the DDD. Table 2 illustrates the prescription of lipid-lowering drugs in patients with T2D who did not reach target LDL-C levels across various provinces.
The results indicate that prescribing lipid-lowering drugs was not appropriate for the patient’s needs in the selected provinces. This inadequacy included no medication and insufficient medication therapy for patients with high LDL-C levels (Table 2).
DISCUSSION
Managing dyslipidaemia in patients with T2D is crucial for reducing the risk of cardiovascular events. This study aimed to evaluate the prescription pattern of lipid-lowering drugs, identify medication errors, and assess the achievement of individualised targeting levels. The results shed light on the current state of lipid control in patients who are diabetic in Iran, and highlight areas for improvement.
The treatment of diabetic dyslipidaemia involves both pharmacological and non-pharmacological interventions.5,12,27 It is important to note that lifestyle interventions and medication therapy can reduce the risk of cardiovascular events.28 However, this article aims to evaluate the quality of medical care for blood lipid control in patients with T2D in Iran.
Drug treatments for diabetic dyslipidaemia comprise statins, cholesterol absorption inhibitors, niacin, fibrates, bile acid sequestrants, PCSK9 inhibitors, and omega-3 fatty acids.27,29,30 Statins are commonly used to prevent primary and secondary cardiovascular events. They are effective in lowering LDL-C levels and increasing high-density lipoprotein cholesterol levels.
The Achievement of Individualised Targeting
LDL-C levels across all provinces declined during the 5-year study. However, results show that with an individualised approach, only 26.06% of monitored patients reached their LDL-C targets. This is similar to the DA VINCI study, which found that only 21% of very high-risk patients (including most with diabetes) achieved the guideline LDL-C target (<55 mg/dL).31 According to the ADA guidelines, which recommend an LDL-C goal of 100 mg/dL for patients with diabetes, over 70% of patients reached the lipid control target.17
The most striking finding is the high percentage of patients failing to meet their LDL-C targets across all risk categories.
In 2017, 70.6% of all patients had uncontrolled LDL-C levels. While this is a slight improvement from 73.9% in 2013, it remains unacceptably high. The situation is most critical in the highest-risk groups. For ‘very high’ risk patients, over 92% were uncontrolled in 2013, and this improved only marginally to about 90% in 2017. This ‘treatment gap’ is a global phenomenon. A review study highlighted that despite well-established guidelines, a significant majority of high- and very high-risk patients worldwide fail to achieve LDL-C goals.32
The authors’ data highlight a clear ‘risk-paradox’, showing that patients requiring the most aggressive lipid-lowering treatments are the least likely to reach their targets. In 2017, the low-risk group achieved an 86% control rate, whereas the very high-risk group had only about a 10% control rate that year. Studies that analysed data from millions of patients also found this exact paradox.33,34 These studies suggest that the more aggressive the target (e.g., <55 mg/dL), the more challenging it is to achieve.
The data in Table 3 show that while there was a slight increase in control rates from 2013 to 2017 (overall from 26.1% to 29.4%), the progress is minimal, especially among the highest risk groups. This indicates that the management strategies used during this period were not aggressive enough.
The average LDL-C levels vary across the five provinces. For example, Mazandaran consistently shows higher average LDL-C levels across most risk categories compared to other provinces like Tehran or Kurdistan. Regional variations in cardiovascular risk factors are well-documented and are often linked to differences in diet, lifestyle, socioeconomic status, and access to healthcare services.35
This clearly demonstrates the superiority of the individualised approach in managing dyslipidaemia in people with diabetes.
The difference between provinces is strongly correlated with their population distribution in each risk group (Table 3). That means provinces with the worst cholesterol control have the highest population percentages in very high-risk groups.
Prescription Patterns and Drug Dosage
In most guidelines, if the target LDL-C level is not reached with the maximum tolerable dose of statins, the addition of another drug class, such as ezetimibe or PCSK9 inhibitors, is recommended.1 However, ezetimibe was rare in the study population, and PCSK9 inhibitors were not used. This suggests that physicians have not prescribed lipid-lowering drugs based on LDL-C levels and guidelines for patients with diabetes (Table 2). It also indicates the use of nearly identical prescription patterns for all patients, regardless of their individual needs.
Approximately 23% of patients with uncontrolled LDL-C levels received no medical treatment to lower their blood lipids. Additionally, 17.6% of the patients who did receive medication were not prescribed adequate doses (Table 2). These highlight the inadequate and low-quality care for patients with diabetes in selected provinces of the country. Therefore, it is crucial to take adequate measures to improve the performance of the medical staff, such as providing continuing medical education and developing evidence-based guidelines to enhance the quality of diabetes management.
Effectiveness of Medications
The effectiveness of lipid-lowering drugs was assessed by comparing the LDL-C reduction in patients taking atorvastatin for 2 years with a control group. The results of the authors’ retrospective cohort showed that the mean effectiveness of atorvastatin tablets (10, 20, and 40 mg) was a reduction of 11.56%, 10.13%, and 7.76% in LDL-C levels, respectively (Table 4). However, the effects were not directly related to the prescribed doses, and the level of blood-lipid reductions was lower than expected.25,26
Moreover, the findings show that about 60% of patients with diabetes in the provinces who did not meet the target LDL-C levels had been prescribed a proper DDD of atorvastatin. This indicates that patients either received fewer effective medications, needed higher doses, had to change their lifestyles, or experienced a combination of these factors. More research is necessary to verify each of these possibilities.
CONCLUSION
This study sheds light on the current state of lipid control in patients with T2D in Iran. It provides a stark, data-driven snapshot of the challenges in managing cholesterol in patients with diabetes.
Most people, especially those at the highest risk for heart attacks and strokes, are not getting enough treatment to meet evidence-based targets.
The prescribing pattern of lipid-lowering drugs was suboptimal, with a high rate of medication errors. The rate of achieving individualised LDL-C target levels was low, and the effectiveness of the prescribed medications fell short of expectations.
These findings emphasise the need for improved evidence-based prescription practices, enhanced medical staff performance, continued medical education, and better medication management to ensure improved lipid control in patients with T2D.
LIMITATIONS
This study has some limitations. Initially, the authors did not directly measure the patient’s adherence or compliance. However, since they selected patients with 5 years of complete medical records and at least four doctor visits per year, the authors estimated their adherence was over 70%. The authors also did not evaluate the patients’ kidney health or the toxicity of the drugs used in this study, which could influence the medication’s effectiveness.







